We focus on understanding how changes at the cellular level in skeletal muscle affect muscle structure and function, and, in turn, how pathological changes in muscle affect cellular processes.
Follow @lab_meyer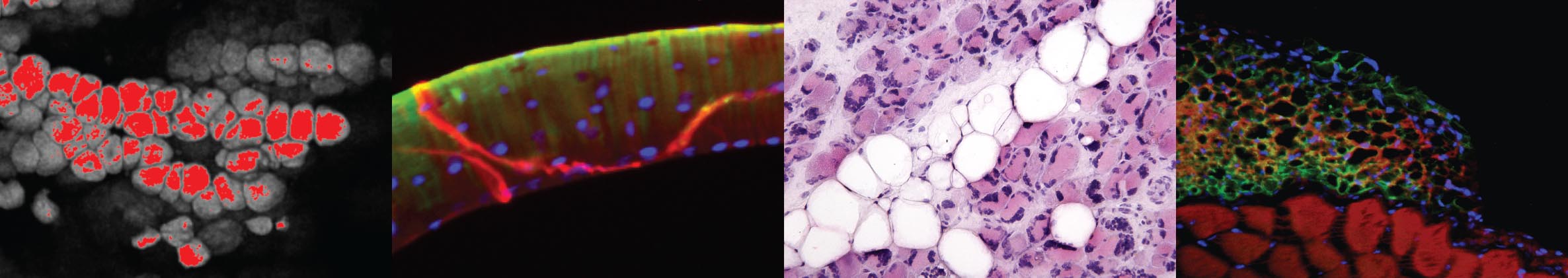
At any given time, muscle tissue houses 5-10 distinct populations of cells, all of which communicate with each other and with their environment to regulate homeostasis and ensure proper muscle function. We know that when something goes awry, as in injury or disease, this communication gets interrupted or misdirected, and cells, such as fibroblasts and adipose progenitors, respond inappropriately by replacing healthy muscle tissue with connective tissue and fat. Yet we don’t fully understand the “language” of these cells, and this keeps us from being able to fully restore cellular interaction and tissue function in many pathologies.
Our main projects are focused on the interaction between muscle and fat. Though much less studied than its “pathological sibling”, fibrosis, the formation of fat in and around muscle is equally prevalent across myopathies. Our research investigates fat’s effect on muscle function and how that effect is regulated at cellular and tissue levels.
Current Lab Members

Faculty Investigators
Gretchen A. Meyer, PhD [Profile ![]() ]
]
Staff and Student Members
Jeremie Ferey, PhD
Lab Manager
Jake Parson
Ph.D. Student, Movement Science
Chang Gui
Ph.D. Student, Biomedical Engineering
Dakota Kamm
Ph.D. Student, Movement Science

Karen Shen
Research Technician
Cameron Swick
DPT Student
Current Research Studies
The functional consequences of fat accumulation in muscle

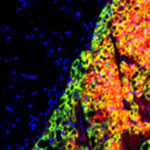
Decellularized muscle was stained with BODIPY, imaged with confocal microscopy and digitally reconstructed to generate this 3-D map of intramuscular fat.
The accumulation of adipocytes within skeletal muscle is a nearly ubiquitous feature of muscle pathology – associated with conditions as diverse as aging, diabetes and tendon injury. Though this fat accumulation is frequently associated with poor muscle strength in humans, a direct link has not been established due to systemic disease pressures that simultaneously affect muscle cells. Recently, we have developed methodology for high-resolution mapping of intramuscular adipocytes in mouse muscle that we are using in conjunction with precision ex-vivo analysis of muscle contractile performance to define the direct effect of fat accumulation on muscle function. Ongoing work in this area is investigating the effect of fat accumulation on hypertrophic signaling and the potential for dynamic forces (resistance exercise) to reverse this pathology.
Check out https://pubmed.ncbi.nlm.nih.gov/32358797
The role of fat phenotype in fat-muscle cross-talk
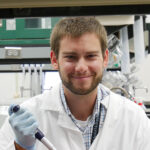
A transplanted graft of brown fat next to the supraspinatus muscle of the rotator cuff stained for perilipin (green) and UCP1 (red).
The way we think about the function of fat in the body has changed dramatically over the past 10 years. Fat is now recognized as one of the most important endocrine regulators of body physiology – affecting a diversity of cells from neurons to osteoblasts. However, despite the close proximity of muscle and fat (specifically inter-muscular adipose tissue – IMAT), we know very little about how these tissues might signal each other locally. To explore this important question, we have developed an inter-muscular fat transplant model in the mouse where we can alter fat phenotype and genotype to study the factors that influence fat-muscle cross-talk. Ongoing work on this project is exploring the role of brown and browned-beige fat signaling on muscle degeneration and regeneration in the rotator cuff. It is our hope that defining these interactions will lead to fat-targeted therapies in rotator cuff tears where excessive accumulation of beige fat is impeding muscle functional recovery.
Check out: https://www.ncbi.nlm.nih.gov/pubmed/?term=31042310
The cellular basis for poor muscle performance in diabetic peripheral neuropathy
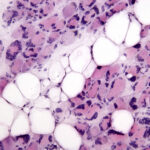
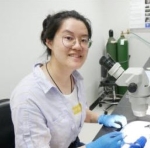
Histological image of a biopsy from an individual with diabetic peripheral neuropathy demonstrating fat infiltration (white circles).
The accumulation of intramuscular fat is dramatic in diabetic peripheral neuropathy – replacing as much as 90% of the volume of muscles of the foot and calf. To better understand the interaction between these intramuscular adipocytes and neighboring muscle fibers in humans, we are obtaining biopsies from participants undergoing amputation, separating the muscle and fat components and isolating progenitor cells. Using these cells we can generate patient-specific co-culture models to study paracrine secreted factors from intramuscular fat and how those signals regulate myogenesis.
Check out: https://pubmed.ncbi.nlm.nih.gov/32059624/
Guiding cell-based therapies to prevent fibrosis

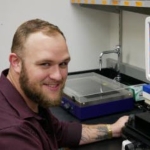
An APC immunostained for actin (green) and YAP (red). Defined actin stress fibers and nuclear YAP localization are typical of APCs grown on stiff substrates. These cells secrete more connective tissue matrix and exhibit signs of switching to a pro-fibrotic myofibroblast phenotype.
Post-transitional control of EC-Coupling
We are embarking on a new project to understand how EC-coupling is regulated by post transitional modifications. We have evidence that acetyltransferases p300/CBP are critical for muscle contraction, but the mechanism has yet to be determined. Check out http://pubmed.ncbi.nih.gov/31898871/. Our preliminary data support post-translational acetylation of protein(s) involved in EC-coupling can be tested in isolation to prove this and further hone the mechanism. You could be the one to figure it out! Apply to a post-doc with us today!