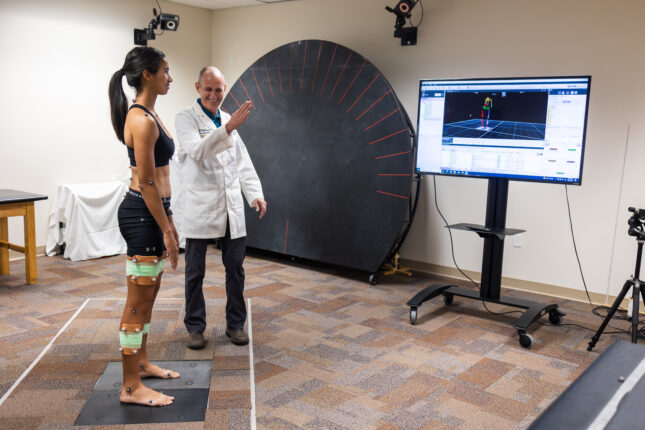
The goal of our work is to understand how the musculoskeletal and nervous systems interact to contribute to the development of musculoskeletal conditions across the lifespan. We also are interested in how psychosocial and environmental factors impact these interactions.
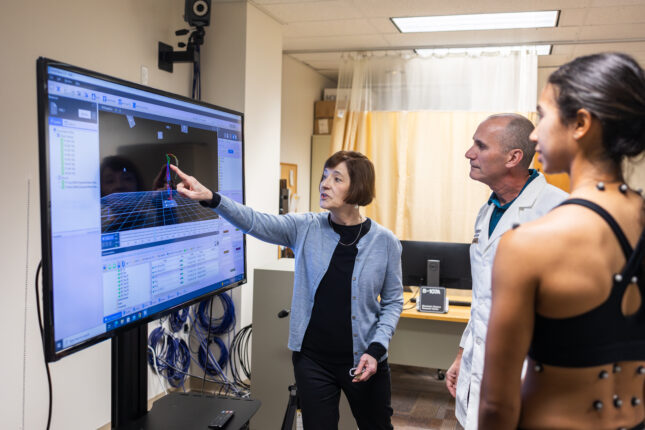
Musculoskeletal conditions are among the most disabling and costly conditions experienced by Americans and are the leading cause of physical disability in the United States. Treatments that prevent or lessen the long-term impact of these conditions are needed. Our major funded studies have focused on low back pain (LBP) conditions. These studies have included testing the reliability and validity of a classification system for non-specific LBP as well as understanding the relationships between posture and movement characteristics and variables such as symptoms, sex, activity demands, and neural and musculoskeletal factors. We also have examined the efficacy of different non-surgical treatments for people with chronic LBP and explored the role of adherence on short- and long-term outcomes. Our current work is focused on understanding the role of movement-related impairments found to be important in chronic LBP conditions, to the course of acute LBP.
Faculty Investigator
Linda Van Dillen, PT, PhD, FAPTA [Profile ![]() ]
]
Vanessa Lanier, PT, DPT, OCS [Profile]
Staff
Chris Peterson, PT, DPT, OCS
McKenna Chapman, BS
Billie Jacobsen, BS
PhD Trainees
Kayla Krueger, PT, DPT
Other Trainees
Amy Kang, SPT
Mo Moeslein, SPT
Lauren Marshall, SPT
Current Funding and Collabortions
- NIH/NICHD RO1 HD108240: Significance of Spinal Movement Impairments in Acute Low Back Pain
- Academy of Orthopedic Physical Therapy, APTA P19-03313: Impact of Hip Structure and Function on the Clinical Presentation of Low Back Pain
Current Research Studies
Significance of Spinal Movement Impairments in Acute Low Back Pain
The course of recovery from acute LBP is variable and many people have incomplete recovery. We are going to examine people with an acute episode of low back pain. We will identify movements and postures that may or may not be associated with recovery, and if they are similar to the impairments that were previously identified as relevant to the course or recovery in people with chronic low back pain. The participants will be followed to see who recovers and who develops chronic low back pain. This information will help determine if person-specific movements and postures used during function might be a clinical biomarker for recovery from acute low back pain and a potential treatment target for those who are at risk of incomplete recovery to improve the long-term course of the back pain condition.