Our multidisciplinary research team is committed to improving quality of life for individuals living with shoulder pain associated with conditions such as rotator cuff tears and osteoarthritis. We seek to develop improved treatment strategies by understanding the factors underlying the pathology, symptom manifestation, and functional decline. Our approach is to conduct rigorous, clinically relevant research that integrates clinical assessment, diagnostic imaging, and state-of-the-art methods of assessing the human movement system with the passion and expertise of a multi-disciplinary research team.
Faculty Investigator
Current Research Studies
“Investigating the Multi-factorial Etiology of Rotator Cuff Pathology in Human Subjects“
A rotator cuff tear is a common shoulder condition affecting approximately 40% of individuals over the age of 60. This condition is often painful, debilitating, and impairs quality of life. Despite their prevalence, the cause of rotator cuff tears is not fully understood but is generally believed to involve extrinsic factors (i.e., tendon impingement during shoulder motion), intrinsic factors (i.e., tendon degeneration), and overuse. These factors have been studied extensively in animal models, which have provided support for each factor contributing to rotator cuff pathology and, perhaps more importantly, that a combination of factors may be more impactful than any individual factor. Therefore, the objectives of the proposed studies are to: 1) develop a preliminary multivariable model classifying the effects of extrinsic, intrinsic, and overuse factors on rotator cuff pathology in asymptomatic individuals (K99); 2) extend the model with additional asymptomatic participants (R00); and 3) expand the model to include symptomatic participants (R00).
Funding: NIH/NIAMS (K99-AR075876, R00-AR075876)
Check out: https://pubmed.ncbi.nlm.nih.gov/34636897/, https://pubmed.ncbi.nlm.nih.gov/32807327/, https://pubmed.ncbi.nlm.nih.gov/35880416/
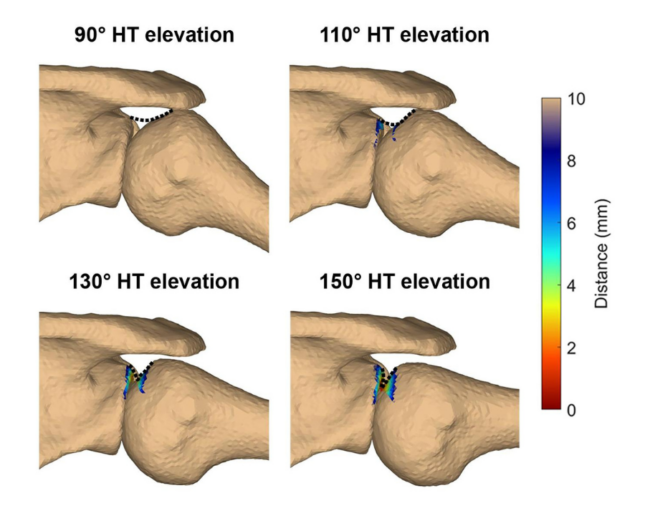
“Determine the impact of simulated scapular movement impairments on mechanisms of rotator cuff tendon injury“
Scapular movement impairments are often observed in individuals with shoulder pain and have been hypothesized as an underlying cause of rotator cuff pathology. For example, movement impairments (e.g., insufficient upward rotation) are believed to impact the frequency or magnitude of rotator cuff impingement, which can occur during shoulder motion when the rotator cuff tendon becomes abraded under the coracoacromial arch (subacromial impingement) or entrapped against the glenoid (internal impingement). However, the impact of scapular movement impairments on these potential mechanisms of tendon injury remain unclear. Therefore, this study aims to determine the extent to which simulated changes in scapular kinematics impact the acromion-to-footprint (subacromial) and glenoid-to-footprint (internal) distances.
Check out: https://pubmed.ncbi.nlm.nih.gov/30658048/, https://pubmed.ncbi.nlm.nih.gov/31377124/
“The Biomechanics of Eccentric Glenohumeral Osteoarthritis“
Eccentric glenohumeral osteoarthritis (GH OA) is a unique pathology that remains poorly
understood. While the combination of posterior humeral subluxation and asymmetric glenoid
erosion has been well-described, the cause of eccentric GH OA remains unknown. This gap in
our knowledge is consequential because clinical management of these patients is especially
challenging as evidenced by higher rates of surgical complications and poorer patient-reported outcomes. Thus, the long-term goal of our multidisciplinary research team is to improve clinical outcomes of patients with eccentric GH OA by understanding the mechanisms underlying the development and progression of joint degeneration.
Funding: OREF/ASES/Rockwood Shoulder Grant
“Developing and Validating Low Dose CT Protocols for Research and Clinical Applications“
Computed tomography (CT) scans are the gold standard modality for creating 3D
reconstructions of bony anatomy. The resulting bone models are used in numerous research
applications including geometric analysis, model-based kinematic tracking, and musculoskeletal models. However, CT imaging exposes patients and research participants to ionizing radiation, yet lower dose protocols are likely possible given the high natural contrast between bone and surrounding tissues. We recently determined that radiation dose can be reduced by up to 92% without substantially impacting the accuracy of 3D geometric reconstructions or 3D kinematic tracking. Our team is now working to translate these low dose protocols into clinical practice, first in patients following glenohumeral dislocation.
Funding: NIH/NIAMS (R00-AR075876) and OREF Resident Research Project Grant
Check out:
https://pubmed.ncbi.nlm.nih.gov/39505762/
https://pubmed.ncbi.nlm.nih.gov/39160033/
Current Lab Members

Stacey Chen, PT, DPT, ATC
PhD student, Movement Science

Anna Spracklin
PhD student, Movement Science

Lydia Nicholson
Research Assistant, BS student in Biomedical Engineering

Sarah Baldwin
Research Assistant, BS student in Biology (pre-PT)

Ashlynne Allen
Clinical Research Assistant II

Nicholas Seifried
Research Assistant, BS student in Neuroscience, Applied and Computational Mathematics and Statistics at the University of Notre Dame

Brooklin Sachs
Research Assistant, BS student in Biomedical Engineering

Connor Dechiro
Clinical Research Data Assistant
Past Members
2023 – Kevin Roseni, research assistant
2023 – Erin Lee, visiting pre-doc researcher in Mechanical Engineering, Queen’s University
2023-2025 – Tessa Roberts, clinical research assistant
2023-2025 – Samantha Loudermilk, DPT research assistant
Collaborators
- Marcie Harris-Hayes, PT, DPT, MSCI; Program in Physical Therapy, WashU Medicine
- Renee Ivens, PT, DPT; Program in Physical Therapy, WashU Medicine
- Jay Keener, MD; Department of Orthopaedic Surgery, WashU Medicine
- William Middleton, MD; Department of Radiology, WashU Medicine
- Kelby Napier, MD, PhD; Department of Radiology, WashU Medicine
- Michael Rainbow, PhD; Department of Mechanical and Materials Engineering, Queen’s University
- Steve Soliman, DO, RMSK, FAOCR; Division of Musculoskeletal Radiology, University of Michigan
- Sharlene Teefey, MD; Department of Radiology, WashU Medicine
- Benjamin Zmistowski, MD; Department of Orthopaedic Surgery, WashU Medicine