The Tendon Rehabilitation Lab is committed to improving care for people with tendon injury and dysfunction. Our research is aimed at advancing our understanding of person-specific factors that affect a tendon’s ability to respond to treatment. This includes local factors, like tendon structure, and systemic factors, like the presence of diabetes.

Tendons connect muscles to bone and are critical for transferring muscle forces into efficient movement. One of the best available treatments for tendon injury is to gradually increase the loads placed on the tendon so that the tendon receives the signals needed to heal. While progressive tendon loading is the recommended standard of care, there is a need to further clinical decision-making and improve treatment options for people with tendon dysfunction. Optimizing care is important because tendon recovery regularly takes months, recurrent injury is common, and response to tendon loading varies from person to person.
The Tendon Rehabilitation Lab’s vision is to optimize treatment for tendon dysfunction by personalizing dosing of tendon loading and aligning adjunctive treatments to give the tendon the environment and signals it needs to recover. Our approach to answer these tendon questions combines clinical performance measures, diagnostic imaging, and basic science methods.
Faculty Investigators
Jennifer A. Zellers, PT, DPT, PhD
Lab Members

Yi Kang, DPT
Graduate Student
Movement Science Program

Rachana Vaidya, PhD
Postdoctoral Research Associate
CV
Sophiae McSpedon
Research Assistant
Gary Wang
Research Assistant
Kade Ariano
Research Assistant
Adriana Britto-Pereira
Undergraduate Researcher
Current Projects
Effect of Metabolic Syndrome on Achilles Tendon Structure and Function

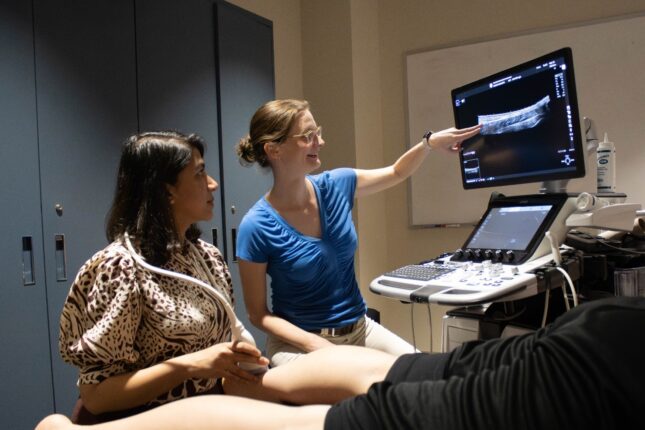
Eighty percent of people attending outpatient physical therapy have diabetes, pre-diabetes, or diabetes risk factors. People with metabolic syndrome are at 2-3x greater risk for developing tendon injury. Despite the clinical implications of metabolic syndrome on tendon tissue, relatively little is known about how metabolic syndrome affects tendon health and recovery from injury. In these studies, we are examining the effect of metabolic syndrome on tendon tissue using a combination of in vivo and ex vivo approaches in humans and preclinical models. This includes basic science tools like tensile mechanical testing and composition assessment, in collaboration with labs in Mechanical Engineering & Materials Science, the Department of Orthopaedics, and the Shared Proteomics Core Resource (supported by the Musculoskeletal Research Center Pilot & Feasibility Award and ICTS Just-In-Time funding). This study is also looking at tendon characteristics of individuals with metabolic syndrome in vivo using modalities like quantitative ultrasound imaging and MRI.
Funding: NIH K01 AR083496 (PI: Zellers)
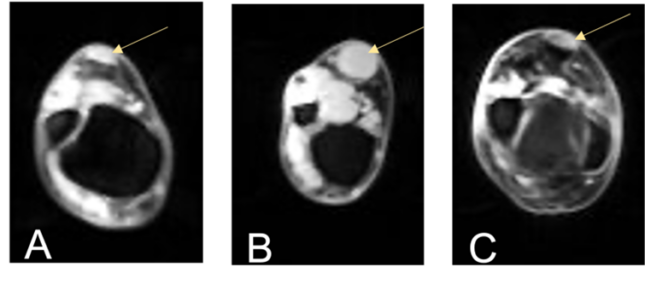
Application of Diagnostic Imaging Modalities to Characterize Tendon Tissue
Quantitative ultrasound and MRI show promise in characterizing tendon tissue. Continued research is focused on how to optimize these techniques and incorporate them into clinical decision-making.

Our projects in this area aim to improve our understanding of the clinical implications of quantitative ultrasound and MRI metrics. We do this by comparing diagnostic imaging metrics to measures of tendon structure in ex vivo tendon specimens. We are also investigating using diagnostic imaging measures dynamically during tasks like a heel-rise to better understand how the tendon moves during functional tasks. This project is in collaboration with laboratory groups in the Mallinckrodt Institute of Radiology.