(Last Updated for AY 25/26)
Welcome Future Doctors of Physical Therapy to WashU Medicine Physical Therapy!
You were selected as one of our learners because of our confidence that, with your achievements and future potential, you will succeed in this program. The physical therapy profession is a dynamic one, with recent changes in health care and laws providing physical therapists with ever-encouraging and exciting opportunities for practice. Individuals entering this doctoring profession are truly those who care about furthering science and the health of the society. We are fully committed to your becoming a physical therapist and the faculty welcomes you into our profession.
As a learner in physical therapy, you will gain knowledge, technical skills and professionalism training that will prepare you for entry-level practice as a physical therapist. This requires more classroom hours than might be the case in a non-clinical graduate program. To ensure your success in completing this challenge, the program, its faculty members and learners must all take certain responsibilities.
The Program will
- provide a wonderful educational environment, where we are all able to teach, learn, conduct research, treat patients, and contribute to the university and the profession. We are grateful for the resources we have for faculty and learners, all of which facilitate the teaching and learning process.
- support the delivery of a curriculum that fosters the development of critically-thinking, competent general practitioners who are well versed in the examination, diagnosis and treatment of the movement system and can deliver quality health care in a variety of settings and meet the challenges presented in clinical practice
The Faculty will
- plan, design, and implement learning experiences that allow learners to achieve the program’s objectives.
- remain actively involved and current in patient care, conducting research, publishing their work, and contributing to the university and the profession.
- access other individuals at the University and in the community to aid us in our endeavors as faculty members.
The Learners will
- take individual responsibility for their own education and their investment for the future.
- work together as a team to benefit most from their education.
- participate in a spirit of cooperation with faculty.
- represent the Program professionally in all venues.
Our learning environment
The Program in Physical Therapy at WashU Medicine creates a learning environment for the DPT curriculum that promotes the health and equity of learners, employees, and members of our community. We believe that the ideal learning environment is created when learners are immersed in academic physical therapy and surrounded by professionals engaged across the triple aim of education, research, and clinical practice. Our learners work collaboratively with expert clinicians immersed in the contemporary clinical environment, top researchers in physical therapy and medicine who incorporate new discovery in the classroom, and master educators who integrate new knowledge through the best practices in the learning sciences.
The curriculum is structured by adhering to these guiding principles, which are informed by the science of learning.
- Use movement and the movement system as the foundations for content selection, organization, and integration
- Create a learning environment that supports the development, health, and wellness, of the master adaptive learner
- Coach and mentor all learners throughout the curriculum
- Provide a diverse set of active learning activities
- Incorporate situated learning experiences early and often
- Apply an assessment framework that is competency-based and learner-centered
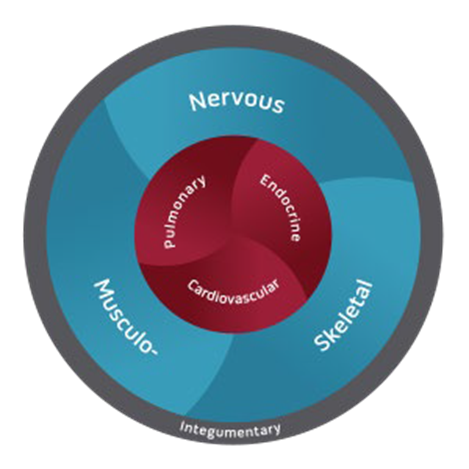
Movement is at the core of our mission, and the human movement system is the foundation of our profession. The human movement system is a system of physiological organ systems that interact to produce and support movement of the body and its parts. Physical therapists are movement system experts.
Human Movement System
WashU Medicine Physical Therapy will lead in advancing human health through movement, integrating interdisciplinary research, outstanding clinical care and education of tomorrow’s leaders to drive optimization of function across the lifespan.
Education
- Prepare exceptional practitioners and researchers who contribute to the practice and science of physical therapy by providing education exclusively at the doctoral level and using innovative teaching strategies delivered by expert faculty. We:
- Prepare clinical leaders who are practitioners of choice in diagnosis-based patient care and who aspire to exceed accepted standards for compassionate care and promotion of health.
- Provide creative post-professional education that enable physical therapists to achieve advanced knowledge, skills and effectiveness in health care delivery
- Develop scientists whose research extends the body of knowledge in the movement sciences and whose interdisciplinary work enables translation of new knowledge to enhance clinical practice.
Clinical Practice
The mission of the Clinical Division is to provide high quality, evidenced-based care with compassion. As movement system experts, we strive to diagnose movement impairments and deliver individualized treatment to optimize physical function, health, and wellness across the lifespan.
Research
The mission of the Research Division is to understand a) how the movement system is affected by disease, injury, lifestyle, development, and aging, and b) how movement can be used to promote health by enhancing physical function, activity, and participation across the lifespan. Our interdisciplinary scientific endeavors include mechanistic and translational investigations at all levels of organization from the cell to society.
In advancing human health through movement, WashU Medicine Physical Therapy will:
- Transform our professional identity by promoting the human movement system as the foundation of physical therapy
- Synergistically align creative education, groundbreaking team science, and innovative evidence-based practice within the framework of the human movement system
- Foster a culture of committed common interest that supports diversity, inclusion, critical thinking and creativity
- Embrace consumer values and goals
In concert with the view of the University and the School of Medicine, the Program in Physical Therapy strives to create a collaborative learning environment in which each physical therapy learner acquires the knowledge, skills, and attitudes required to practice as an effective and compassionate health care practitioner at the highest level of excellence in a constantly changing health care environment. At the core of the learning environment is a curriculum based on the faculty’s beliefs about clinical practice and the profession of physical therapy. These beliefs are:
- Physical therapists have unique expertise and are the practitioners of choice in the areas of prevention, diagnosis, prognosis, and treatment of movement-related conditions;
- Physical therapists have a responsibility to promote optimal movement and general health and to prevent injury, disability, disease and loss of function;
- Clinical practice is based on the clinical science of physical therapy, a body of knowledge drawn from the basic biomedical and physical sciences, applied and clinical research evidence regarding specific movement-related conditions in humans, expertise regarding clinical phenomena, and knowledge of human behavior derived from the social and behavioral sciences;
- Optimal clinical effectiveness depends upon the ability of clinicians to think critically; to make decisions in accordance with the current best evidence, sound clinical judgment, and patient preferences; and to function autonomously in a collaborative, collegial manner with other health care practitioners;
- Physical therapists must perpetually pursue life-long personal and professional development to enhance their ability to assume multiple and continually changing roles required of health care professionals who are leaders in a dynamic health care environment.
The primary goal of the professional curriculum is to prepare physical therapists who are committed to providing skillful, evidence-based practice, and continuing growth and development of themselves and the profession.
WashU Med PT DPT graduates embrace their professional identity as leaders in their community, dedicated to advancing human health by preventing, diagnosing, and managing movement problems across the lifespan.
Our domains of competence are the broad, distinguishable areas of competence that together constitute the general descriptive framework for the profession and our program. Each learner will progress towards competence in each of these areas as they move through the curriculum.
Patient and Client Care (PCC)

Provide informed, effective, and efficient care for the management of movement problems and the promotion of health and wellness.
PCC 1 Obtain a history including review of systems
PCC 2 Decide whether physical therapy is/is not indicated and, make referrals, as needed
PCC 3 Recognize emergent or unsafe situations and take action
PCC 4 Perform a systems review to guide examination
PCC 5 Perform a systematic examination; use and interpret tests and measurements appropriate for movement problems
PCC 6 Make a diagnosis within the profession’s scope of practice based on the synthesis of all patient or client data
PCC 7 Make a prognosis based on the diagnosis and other factors that moderate an individual’s outcome
PCC 8 Make evidence-informed decisions about interventions based on the diagnosis and prognosis
PCC 9 Perform interventions safely, accurately, and efficiently
PCC 10 Promote health and wellness by providing services aimed at preventing movement problems
PCC 11 Provide direction and supervision of students and support personnel
Knowledge for Practice (KP)

Integrate knowledge from established and evolving movement and other relevant biomedical, clinical, epidemiological and social-behavioral sciences to guide practice
KP 1 Apply knowledge of movement science that is fundamental to guiding the management of movement problems
KP 2 Apply knowledge of relevant biomedical sciences that is essential for the care of patients and clients
KP 3 Apply knowledge from clinical sciences to diagnostic and therapeutic decision-making, clinical problem-solving, and other aspects of evidence-informed health care
KP 4 Apply knowledge from epidemiological sciences to the identification of health problems, risk factors, treatment strategies, resources, and disease prevention/health promotion efforts for patients and clients
KP 5 Apply knowledge from social-behavioral sciences to provision of patient and client care, including assessment of the impact of psychosocial and cultural influences on health, disease, care seeking, care compliance, and barriers to and attitudes toward care
Practice-Based Learning and Improvement (PBLI)

Evaluate one’s delivery of care, appraise and assimilate scientific evidence, and continuously improve performance based on self-evaluation
PBLI 1 Integrate self-reflection and external feedback to identify strengths, deficiencies, and limits in knowledge, skills, and attitudes
PBLI 2 Determine one’s learning and improvement goals to enhance outcomes across varied practice settings and diverse patient and client populations
PBLI 3 Address gaps in knowledge, skills, and attitudes by engaging in learning experiences
PBLI 4 Implement changes in practice using systematic quality improvement methods
PBLI 5 Appraise new and existing guidelines, standards, technologies, products, or services; implement and disseminate as appropriate.
PBLI 6 Assimilate and implement best available evidence related to health and movement problems in individuals, communities, and populations
Interpersonal and Communication Skills (ICS)

Use effective interpersonal and communication skills to interact and collaborate with others
ICS 1 Adapt to a variety of verbal and nonverbal communication styles during interactions with patients and clients
ICS 2 Write precisely and intelligibly
ICS 3 Use communication tools and technologies as specified by the organization
ICS 4 Communicate effectively with people from diverse backgrounds and experiences
ICS 5 Communicate effectively with colleagues from one’s own profession, as well as, individuals from other health professions and from health-related agencies.
ICS 6 Use negotiation skills to help resolve conflicts
ICS 7 Demonstrate sensitivity, honesty, compassion, respect, and empathy, especially in conversations about difficult topics
Professionalism (PROF)

Adhere to ethical and legal principles, model professional behaviors, and display a commitment to citizenship within the profession and the community
PROF 1 Adhere to the ethical principles of the profession
PROF 2 Obey laws, policies, and regulations
PROF 3 Adhere to the core values of the profession
PROF 4 Demonstrate responsiveness to patient and client needs that supersedes self-interest
PROF 5 Demonstrate respect for patient and client privacy and autonomy
PROF 6 Demonstrate accountability to patients and clients, society, and the profession
PROF 7 Demonstrate sensitivity and responsiveness to a diverse patient and client population
PROF 8 Engage in professional organizations and activities to promote growth, development, innovation, and change
PROF 9 Advocate for patient and client rights, and for health policies, laws, and regulations that benefit the community and the profession
Systems-Based Practice (SBP)

Function effectively and proactively within evolving systems and environments that contribute to the health of individuals and populations
SBP 1 Adhere to privacy rules, safety guidelines, emergency protocols, and infection control policies
SBP 2 Participate in coordination of patient and client care within the context of various health care delivery settings and systems
SBP 3 Assume the role of consultant
SBP 4 Use system resources to produce documentation that supports the delivery of physical therapy services and to maintain security of patient data
SBP 5 Incorporate considerations of payment models, cost–benefit, and risk-benefit analysis in the delivery of health services
SBP 6 Engage in system quality improvement activities
SBP 7 Participate in the development and implementation of policies to optimize movement, health, and wellness for individuals and populations
SBP 8 Perform administrative and practice management responsibilities commensurate with one’s role, abilities, and qualifications
SBP 9 Educate students, trainees, peers, and health professionals from other disciplines within the context of various health services delivery settings and systems
Interprofessional Collaboration (IPC)
Engage within interprofessional teams as an effective member and collaborative leader
IPC 1 Collaborate with other health professionals to establish and maintain a climate of mutual respect, dignity, diversity, ethical integrity, and trust
IPC 2 Apply knowledge of one’s own role and those of other professions to assess and address the health care needs of patients and clients and to promote and advance the health of populations
IPC 3 Communicate with patients and clients, families, communities, and professionals in health and other disciplines in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health and the prevention and treatment of health conditions
IPC 4 Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable.
Personal and Professional Development (PPD)

Demonstrate the attributes required to engage in lifelong personal and professional growth
PPD 1 Demonstrate the ability to cope with physical, mental and emotional stressors
PPD 2 Manage conflict between personal and professional responsibilities
PPD 3 Practice flexibility, adaptability and maturity in negotiating and adjusting to change with the capacity to alter one’s behavior
PPD 4 Demonstrate trustworthiness that affords opportunities for personal and professional growth
PPD 5 Demonstrate self-confidence that puts patients and clients, families, and members of the health care team at ease while portraying humility and respectfulness PPD 6 Demonstrate the curiosity, initiative, motivation and commitment requisite for lifelong learning
The activities within the Program in Physical Therapy are grouped into three major areas: education, research, and clinical practice. Participation in these three areas enables us to contribute broadly to the advancement of the profession of physical therapy. It is both a privilege and an obligation for the faculty and learners to participate in all three areas.
The organizational charts found in the Canvas Student Commons pages will familiarize you with how the Program is organized. Within this basic structure, you will find the lines of communication to be open and the faculty to be actively concerned that their activities be well integrated into a meaningful whole. This means we have a commitment to your education that is equal to our research and patient care activities.
You have a very dynamic faculty at WashU Medicine. In addition to a core group of faculty members, many other physical therapists and experts in health care are involved in both lecturing and lab assisting.
All core faculty members are involved in teaching, as well as clinical practice and/or research. Most faculty members are involved with the American Physical Therapy Association and other professional societies. Make time to get to know your faculty and their activities. Names of the faculty leads are on the top of each session page.
Staff members are skilled and friendly. You will find many of them working in the main office, the clinical practice, and in the various research laboratories. Please visit this WashU PT Web Page to learn more about faculty and staff members.
The Program in Physical Therapy is accredited by the Commission on Accreditation in Physical Therapy Education (CAPTE), 3030 Potomac Ave., Suite 100 Alexandria, Virginia 22305-3085; telephone: 703-684-2782 or 1-800-999-2782; email: accreditation@apta.org; website: www.capteonline.org.
CAPTE is listed as a nationally recognized accrediting agency by the US Department of Education and the Council for Higher Education Accreditation (CHEA). Once awarded accreditation status, a program must submit reports regularly to the Commission ensuring continuing compliance with the evaluative criteria and is formally reviewed every five to ten years.
The Commission on Accreditation of Physical Therapy Education (CAPTE) governs the specialized accreditation of every physical therapist education program in the USA and some programs in Canada. Our Program has maintained continuous accreditation since 1942. Our last review in 2018 yielded continued accreditation. The next CAPTE visit will occur in March 2028. Each review requires construction of a Self-Study that documents all components of the Program and its professional education curriculum. Careful review of all aspects of the Program, School of Medicine, and University that impact education is key to the decision about whether to reaccredit the Program. All faculty are expected to participate in preparation of the Self-Study (under the direction of the Program Director and relevant Division Directors) and the visit from the On-Site Team assigned by CAPTE to our Program.
Specific policies and procedures associated with maintaining CAPTE accreditation to which the Program continuously complies include:
• Timely submission of required fees and documentation, including reports of graduation rates, performance on state licensing examinations, and employment rates.
• Timely notification of expected or unexpected substantive change(s) within the Program and of any change in institutional accreditation status or legal authority to provide post-secondary education.
• Coming into compliance with accreditation criteria within two years of being determined to be out of compliance.
The only mechanism through which CAPTE can act on a concern is through a formal complaint process. The complaint must be related specifically to one or more of the Evaluative Criteria for Accreditation, or one or more of CAPTE’s expectations related to program integrity. The formal complaint process can be accessed in the Accreditation Handbook, available through the CAPTE web site (www.capteonline.org).
WashU Medicine Program in Physical Therapy does not discriminate against qualified people with disabilities in the admissions process. We do require all students to meet the Program’s technical standards with or without reasonable accommodations. These standards are necessary to allow success during the academic and clinical phases of study, and the capacity to pass licensure requirements and attain future employment. The standards are intended to protect the health and safety of students, faculty, and patients. An offer for admission may be withdrawn if an admitted student is not able to articulate how he or she would meet the program’s goals and objectives, even with accommodation. The faculty expects graduates to be prepared to function in a broad variety of clinical situations and render a wide spectrum of patient care.
The technical standards apply throughout the duration of the curriculum. However, we do use clinical sites that may have different standards or not be able to offer the same accommodations as provided by the Program. Students with questions should call the admissions office at 314-286-1402.
Program faculty, in accordance with the Commission on Accreditation in Physical Therapy and the Standards of Practice in Physical Therapy, identifies the following fundamental skills for our curriculum and for the profession:
- Problem solving on the basis of verbal, visual and written information, within a limited time frame
- Clinical reasoning and decision making within a limited time frame
- Insight and judgment for safety and prognostication
- Visual-spatial integration
- Perceptual motor integration
- Repetitive motion
- Effective communication among group members
- Planning and organizing for treatment prescription
- Frequent lifting, pushing, and pulling up to 20 pounds
- Occasional lifting, pushing, and pulling of 20-50 pounds
- Time management to coordinate course and clinical requirements
The admitted student must possess the following skills and abilities:
Observation: The ability to observe demonstrations and visual aids used in lectures and laboratories. Students must be able to observe patients at varying distances. This requires vision and somatic function.
Communication: A candidate must be able to speak, hear, and observe patients to elicit information, perceive nonverbal communication, describe changes in mood, and sensitively and effectively communicate with and instruct others. Communication will include speech, reading, and writing. Communication with the health care team will be in oral, written, and electronic form, and be effective, efficient, and timely.
Motor Function: A candidate must have sufficient motor function to elicit information from patients through palpation, auscultation, percussion, and movement of limbs and trunk. He or she must be able to provide care to patients that involves exercising, lifting, transferring, and assisting during walking, all while assuring safety for themselves and others. A candidate should be able to provide basic and emergency care for patients. These activities require coordination of movement, equilibrium, and sensation.
Intellectual-Conceptual, Integrative, and Quantitative Abilities: Candidates must be able to use conceptual, integrative, and quantitative thinking abilities to problem solve. He or she must be able to comprehend 3-dimensional relationships, spatial relationships of structures, and use these skills to analyze and apply this information for problem-solving and decision-making. Candidates must be able to organize, prioritize, analyze, and evaluate complex information individually, in small groups, in clinical settings, and within a limited time frame.
Behavioral and Social Skills: Candidates must have the emotional health to fully use his or her intellectual ability, exercise good judgment, complete all responsibilities, self-assess, accept criticism, and assume responsibility for maintaining professional behavior. He or she must be able to develop mature, sensitive, and effective relationships with others. Being able to tolerate physical and emotional stress and functioning effectively is necessary. Candidates must exhibit adaptability and flexibility and be able to function in the presence of uncertainty. He or she must have high levels of compassion for others, motivation to serve, and a consciousness of social values. A candidate must be able to interact positively with people from all socioeconomic and ethnic levels and respect the belief systems of others.
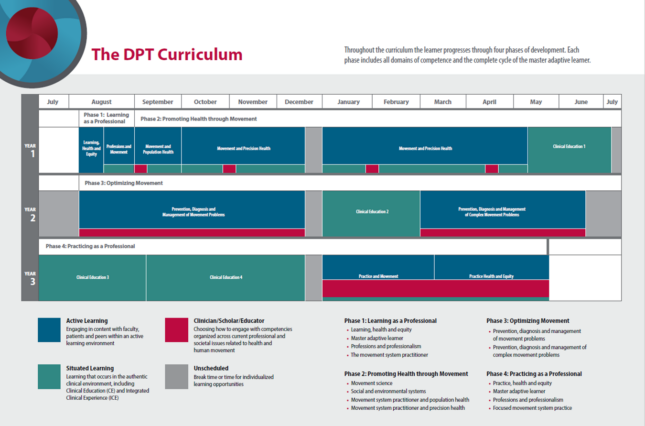
The Program in Physical Therapy at WashU Medicine creates a learning environment that promotes the health and equity of learners, employees and members of our community. The curriculum is divided into 4 phases.
Phase 1: Learning as a Professional
The primary purpose of this phase is to introduce students to the learning environment and the profession through examples focused on health and equity. An understanding of learning science principles, the stages and attributes of the master adaptive learner, and the learning environment for the curriculum will prepare the learner for ongoing personal and professional development. The introduction to the profession will place the emphasis on movement and diagnosis within the historical context of physical therapy.
Phase 2: Promoting Health through Movement
The purpose of this phase is the application of movement science and social and environmental system science to human movement and the continued development of the physical therapist as a movement system practitioner. An emphasis is placed on how health is impacted by movement from the societal to molecular levels. The phase emphasizes health and prevention through movement as a primary role for the physical therapist. The learner is prepared for safe entry into the authentic clinical environment.
Phase 3: Optimizing Movement
The purpose of this phase is the application of the movement system and social and environmental system science to patient client management. An emphasis is placed on direct patient care, which includes all levels of prevention and care (primary to tertiary). Health status and its relationship to movement across the lifespan will be organized within the context of the different health systems.
Phase 4: Practicing as a Professional
The purpose of this phase is to prepare the learner for independent practice and licensure, while allowing for flexibility to focus on areas of interest. Learners return after their final clinical experience to complete the full cycle of the master adaptive learner. Reflection on situated learning provides an opportunity for the learner to identify and address areas of improvement, prepare for the licensure examination, and explore areas of interest or future specialization.
The curriculum contains curricular modules, domains and clinical education courses. Total Credits = 114 credits.
Registration & Tuition
Student registration occurs at the beginning of each semester. Registration is computerized and the Program will register all students prior to each semester unless they have unpaid tuition. Students are responsible for updating their local address and phone number online at the beginning and end of each semester through Workday. You may find additional information on the Workday website at under “Updating your Record” section. Addresses also must be kept current with the DPT Admissions Office via email (PTAdmissions@wustl.edu).
Tuition and clinical fees are billed and payable each semester.
1st Year: Fall/August 30, Spring/January 30 and CE I/May 30,
2nd Year: Fall/August 30, Winter/January 30, Spring/March 30
3rd Year: Summer/July 30, Fall/September 30, Spring/January 30
Your student account may be viewed through Workday, allowing you to access and pay your bill online and to set up direct deposit for refund checks. You may also provide third-party access to family and friends that may be assisting paying for your education. More information can be found on the Workday website under the “Financials” Section. Please note there are some options that are NOT available to medical school students.
Any tuition or fee due and not paid by the specified date may accrue interest at the usury rate in effect on the first business day of the month in which that payment is due. Holds can be placed on the account until the balance is paid in full. A student accounting hold will prevent a student from adding/dropping classes, adding campus card points, and registering for classes. If accounts are not settled, the student will not be allowed to register or attend classes/clinical experiences after that time.
Students who rely on loan or scholarship funds to meet their financial obligations should submit their loan applications for processing at least eight weeks prior to the start of classes each year. The Financial Aid office will assist students with seeking information on financial aid options upon request.
Continuing Student Status
In special instances, the University allows Programs to make the determination that a student can remain with a full-time status, even if units drop under the normal threshold for full-time status. This status is only allowed when a student is registered in an on-going basis in a full-time program, but for some unique reason needs to drop under the full-time threshold. This status allows students to continue with some University benefits, such as student health and the University’s UPass. An individual plan will be discussed with the student if this status is needed. International students are not eligible for the Continuing Student Status.
The Clinical Education Program provides an environment in which the learner is immersed within physical therapy practice. The learner utilizes problem solving and critical thinking skills to integrate specific concepts and techniques into the provision of quality clinical care. This component of the curriculum is comprised of early integrated and full-time clinical experiences, scheduled at a variety of practice settings that represent the broad scope of clinical practice in physical therapy. Each clinical education experience is designed to correlate with the academic preparation of the learner by increasing the number of skills and complexity of problem solving required. The Clinical Education Program promotes a focus on the education of learners to the common practice of physical therapy, which involves professional behavior, communication, patient examination, evaluation, diagnosis, and intervention across inpatient and outpatient settings and with a variety of medical diagnoses. Each learner is expected to actively participate in the clinical education process and to share in the planning and evaluation of learning experiences. In accordance with the commitment of the Program in Physical Therapy to assessing the quality of all activities through internal and external evaluation, the Clinical Education Program incorporates a system of evaluation designed to assess the quality of learner performance, clinical faculty performance, and activities of the Director of Clinical Education/Clinical Education Team.
The clinical education faculty, also known as clinical instructors and preceptors, of the Program in Physical Therapy is regarded as an integral part of the collegial environment in which our learners are educated. The Program is committed to a plan for faculty development for both academic and clinical education faculty that is designed to incorporate a variety of elements leading to professional growth. This exchange of services by the academic and clinical education faculty promotes a cooperative attitude among all involved in the preparation of our future professional colleagues in physical therapy.
The Clinical Education Program is, therefore, an essential ingredient of the curriculum in achieving the goal of producing the type of professional physical therapist who can function competently in general clinical practice. The activities of the Clinical Education Program are supported by the Program as actively as all didactic activities and are recognized as providing the environment in which integration of knowledge, skills, and attitudes occurs as each learner grows into a professional physical therapist. In the final clinical experiences, (consisting of a 10-week and a 12-week rotation), the learner is asked to integrate all knowledge and skills learned in the classroom, laboratory, and prior clinical experiences.
The emphasis during this time is on:
- Complete, accurate and efficient patient evaluation, assessment and diagnosis, including rationale for choice of procedure and concentration on clinical decision making.
- Individualized and creative patient intervention program planning with elements of revision and timely progression of treatments.
- Implementation of treatment plans using effective teaching and communication skills.
- Early planning for discharge and follow-up care.
- Use of evidence in the literature related to examination and intervention.
- Demonstration of professional behaviors such as initiative and assuming responsibilities as appropriate.
- Performance Assessment Criteria for Clinical Education Courses
Performance Assessment for Clinical Education Courses
All clinical education experiences (Integrated Clinical Experience I and II through Full-time Clinical Experience I-IV) are graded on a Pass/Fail basis. The requirements for passing include:
- Achievement of the appropriate rating scale anchors on the PTCPI
- Attendance at the clinical experience and at all class discussion sessions
Additional completion of required learning activities and assessments FOR learning will contribute to the Professionalism Domain of Competence. It is the learner’s responsibility to complete assignments and discuss them with their clinical instructor as needed.
Expectations are explained and distributed for learners and clinical education faculty in advance of each clinical experience. The Clinical Education Team is responsible for evaluating all the requirements for each clinical experience and making the pass/fail decision.
Learners must successfully complete each clinical experience in the order scheduled before proceeding onto the next. In addition, learners will only be permitted to begin a clinical experience if they have met all requirements of the PT CAC.
At any time during clinical experiences, if safety issues, clinical performance, or professional behavior becomes a major concern, a learner may be immediately dismissed by the clinical site personnel or withdrawn from the site and the clinical experience by the Program. This will constitute a failure of that clinical education experience.
Clinical Education Performance Improvement
Under most circumstances, a learner who does not achieve a passing performance in a clinical experience will participate in remediation activities and an additional performance improvement clinical experience. The location, length, and type of this performance improvement clinical experience will be determined by the Clinical Education Team. Learners who are on probation or have extenuating circumstances will be referred to the PT CAC for progression decisions.
Learners who are required to complete a clinical experience performance improvement will incur additional tuition costs at the usual rate. A learner who is unsuccessful on the same clinical education course twice, or who is unsuccessful in more than one clinical education course will be referred to the PT CAC for progression decisions (see PT CAC policies).
Learners requiring additional clinical experience time or those unable to complete all clinical education requirements by module 7 will experience a delay in graduation and eligibility to sit for the National Physical Therapy Licensing Exam (NPTE).
Refer to the Assessment Appeals section for information on appealing a clinical education pass/fail decision.
Early Clinical Experience
Early clinical experience opportunities will occur in the first year of the curriculum as a part of integrated clinical experiences.
Clinical Education I (CE I) and Clinical Education II (CE II)
Both of these full-time clinical experiences are eight weeks long. CE I occurs at the end of the first year of didactic preparation and CE II occurs between modules 5 and 6.
Clinical Education III (CE III) and Clinical Education IV (CE IV)
CE III and IV are the terminal clinical experiences and are 10- and 12-weeks long, respectively. CE III and IV occur following module 6, at the beginning of Phase 4 of the curriculum.
Selection of Clinical Education Facilities
Clinical site selection and development is the responsibility of the Clinical Education Team Members. We presently have over 500 clinical education sites in St. Louis and throughout the United States. In addition, a small number of international clinical experiences are available. Clinical sites are chosen on the basis of their reputation, their philosophy of clinical education, the type of facility, unique opportunities that can be offered to learners, and the clinical expertise or experience of the clinical instructors. Location and travel expenses, for the learner and for visiting faculty members are taken into consideration when a clinical facility is evaluated.
Learners are given the opportunity to request an investigation of a new clinical site. Learners are expected to initiate this through the Clinical Education Team. Learners or family members are strictly prohibited from contacting facilities on their own. The Clinical Education Team will use discretion in choosing the new sites to be investigated depending upon the needs of the learners and of the Program in Physical Therapy. Suggestions for new clinical sites for CE I must be submitted by July 1st of the previous year and suggestions for CE II, III and IV must be submitted by May 15th of the previous year. The time frame allows for site investigation and development of a completed contract prior to the site selection process. It should be noted that learners who suggest a clinical facility will not automatically be placed at that site. All learners have equal opportunity for experiences at any of the sites available.
Appropriate Behavior and Appearance for Clinical Experiences
The physical therapist’s professionalism encompasses not only having specialized knowledge but also being aware of the aspects of behavior and appearance that affect clinical practice. Although there are many variations in both of these latter areas, the requirements below will serve as a basis on which to form your own style of professionalism after graduation. Until then, learners will be expected to adhere to these standards while participating in the clinical education phases of the Program in Physical Therapy or when in contact with patients during other phases of the curriculum.
Appropriate Appearance for Clinical Experiences
Wearing the appropriate attire for both virtual and in-person patient care is important because learners are professional representatives of WashU Medicine. Appropriate attire also provides learners with comfortable, non-restrictive clothing necessary in a physical therapist’s clinical practice. Learners are expected to wear appropriate attire for all activities involving clinical contact with patients. A learner may be specifically requested to change their dress by a clinical supervisor while at that facility. Adapting their style of dress and accessories (including piercings, jewelry and/or false fingernails) to fit the standards set at any facility may be necessary.
Appropriate Attire
The appropriate attire consists of a short white jacket to be worn with professional clothing. This jacket will be provided to each learner as a gift from the Program. The length of shirts/tops should be adequate to cover the entire trunk at rest and during all movements by the learner. That means that no skin should be visible on the abdomen, breasts, or between the shirt and pants when in the clinic. Jeans and t-shirts must never be worn, unless otherwise instructed by the clinical supervisor. Clothing should be in good condition. A nametag, provided upon matriculation, is to be worn on the left side of the jacket below the collar.
Your shoes must be closed-toe style of a neutral color. No sandals, clogs, heels, or other novelty shoes will be permitted. Nylons or socks should be worn. Accessories such as jewelry should be kept at a minimum and should not interfere with treatment or cause potential safety hazards. For example, large earrings or other body rings are inappropriate. Fingernails should be kept short and clean for sanitary and safety reasons. A watch that counts seconds is needed. Hairstyles must stay neat while you work and not interfere with your performance of patient care activities. Long hair should be tied back. Avoid obtrusive hairstyles, and decorative accessories as these could pose a safety concern.
Appropriate Behavior for Clinical Experiences
In addition to employing appropriate social courtesy, the following should be regarded as specific suggestions for professional behavior in the clinical setting:
It is your responsibility to seek all the information you need to be able to comply with the departmental policies in the clinical setting. The orientation given to you by the clinical instructor should assist you in knowing policies, but it is also your responsibility to ask for additional information or seek clarification of information provided. Such policies will concern lunch, breaks, dress code, fire and emergency procedures, departmental hours, and holidays.
Asking questions from your clinical instructor will not only facilitate your learning but will ensure patient safety and quality care. Be discrete about questions asked in front of the patient and reserve all questions regarding prognosis for when the patient is not present. Be aware of your clinical instructor’s time constraints in answering questions as well as your obligation to ask those questions.
Your strict adherence to the ethical standards, which protect the patients’ confidence, is required. Do not discuss your patients’ condition(s) outside the clinical setting. Patients may be discussed with classmates and faculty for educational purposes but avoid identifying them by name.
Your attention to common courtesy is essential in the clinical setting. Communication of respect, your display of good listening skills and sensitive verbal communications will be helpful in promoting productive working relationships with your clinical supervisors and peers.
You are expected to strive toward achievement of the “Professional Behaviors/Generic Abilities” (see handout), displaying appropriate affective/professional behaviors.
Learners are obligated to report back to the school any ethical or legal situations noted at their clinical sites.
Mobile devices may not be turned on during clinic times unless they are being used for an aspect of patient care, and only with permission from the clinical instructor.
Photos/videos should not be taken on personal cell phones or other recording devices.
Learners completing clinical experiences are not allowed to also be employed by the institution/clinic during the time frame of the clinical experience.
Travel for Clinical Education
It is extremely beneficial for learners to have cars; however, a learner may be able to carpool or use public transportation for local clinical experiences. Learners are responsible for their transportation to and from clinical experiences. Additionally, learners must be prepared to travel out-of-town for clinical education. Expenses incurred during local or out-of-town clinical experiences must be paid by the learner. This includes but is not limited to travel (airfare, mileage, and accessibility to transportation), lodging, parking, meals, etc.
Criminal Background Checks
Criminal background checks are required of all incoming learners by WashU Medicine. Learners must clear this background check prior to matriculation into the Program. Subsequent background checks may be required by the clinical sites and/or the Program. The learner will be responsible for any additional costs associated with criminal background checks. No records will be kept by the Program. The Medical School registrar will keep a letter on file stating simply that the learner passed the background check. Minor infractions may be permissible for Program enrollment; however, they may not be permissible by clinical facilities and/or state licensure boards.
Drug Testing
Drug testing is required of all incoming Medical School learners. An 11-panel urine drug test is required prior to matriculation into the program. Learners who do not pass the drug test will undergo further testing by an outside lab. Any learner not passing this test will not be permitted continued enrollment. This includes any future testing required by a clinical facility according to their policies (prior to or during the clinical experience) will need to be completed through the clinical facility or a local agency, at the learner’s cost. Learners who test positive after the first test will be treated appropriately by Learner Health and may be prevented from enrolling in a clinical experience course prior to successful completion of treatment and subsequent clean testing. Clinical facilities may have additional testing requirements beyond those of Learner Health and may also have restrictions for legally obtained prescription drugs. Learners acknowledge that testing positive on a drug test for a clinical experience after matriculation may prevent them from being able to complete the program. Records will be given to the learner and a letter stating the status of their test will be kept through the Medical School registrar.
Insurance and Fees for Clinical Education Experiences
Liability Insurance
Through a self-insured program, WashU protects each duly registered student against lawsuits or claims of medical malpractice. More specific information is provided as part of orientation prior to each clinical period.
Clinical Education Tuition/Fees
Tuition/fees for each session are due no later than the last day of the first month of the experience.
Additional fees associated with clinical education may be needed for student onboarding requirements, travel and housing.
The Medical School Financial Aid Office continues to assist physical therapy students during their clinical experiences, as during the academic class sessions, with financial aid awards and disbursement. If you have any questions, please do not hesitate to contact the office of PT Admissions and Student Affairs or the Medical School Financial Aid Office. Tuition for each session is due no later than the last day of the first month of the experience.
Health Insurance
For detailed information regarding health insurance coverage while in town or away from campus, go to https://studenthealth.med.wustl.edu/students/. In general, if you stay in the St. Louis area for your clinical experiences, your health coverage remains the same: routine care at Medical School Student Health (MSSH), emergency and hospitalization. If your clinical experiences take you outside the St. Louis area, your coverage is for emergency care and hospitalization only (the same as with any time you leave St. Louis for clinical education or for summer break.)
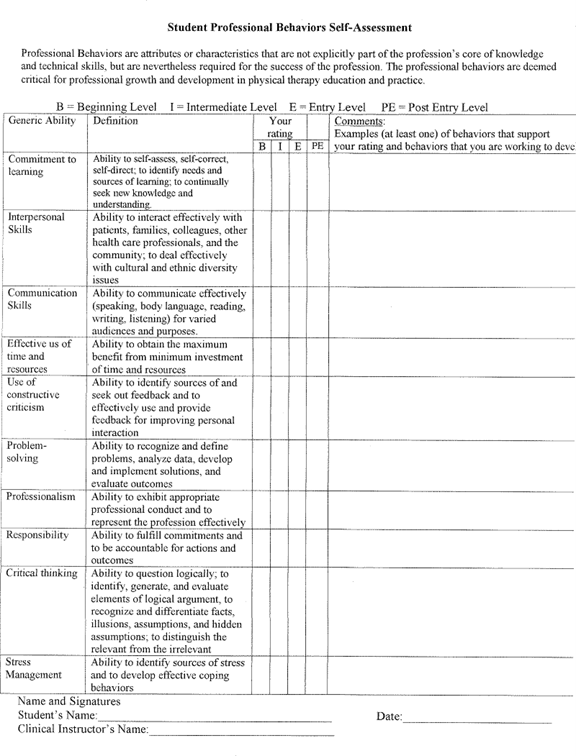
The faculty at the Program in Physical Therapy agrees there are behaviors expected of all learners in a professional program. We have selected as a method of assisting learners to develop professional skills part of a system originally developed at the University of Wisconsin in Madison. The expected behaviors are termed “Generic Abilities”. These abilities are described in detail in the following several pages.
Learners are not expected to automatically demonstrate advanced skills in all areas of the assessment, but basic behaviors are expected from learners at all times, in the classroom and the clinic; and learners are expected to develop as they progress through the program. Learners are expected to become familiar with the information on the generic abilities early in the curriculum.
Self-Assessment: Near the middle of the fall semester, all learners are required to complete a self- assessment of their Generic Abilities using a form developed by the program. The Clinical Education Team Members review the self-appraisals and return them to learner with appropriate feedback as needed. Copies are not retained by the Program. Learners experiencing difficulty in developing professional behavior are expected to assist faculty in identifying ways to further their development
Assessment by Academic Faculty: Faculty may expect learners to demonstrate all or some of the Generic Abilities as part of class participation or during class activities. Faculty will use the descriptions of the generic abilities to communicate with learners about expectations.
Assessment by Clinical Faculty: The Generic Abilities Assessment by clinical faculty and additional self- assessment will occur during the Early Clinical Experience (ECE) and continue into the full time clinical experiences (CE I-IV).
Definitions of Behavioral Criteria Levels
Beginning Level – behaviors consistent with a learner in the beginning of the professional phase of physical therapy education and before the first significant internship
Intermediate Level – behaviors consistent with a learner after the first significant internship
Entry Level – behaviors consistent with a learner who has completed all didactic work and is able to independently manage a caseload with consultation as needed from clinical instructors, co-workers and other health care professionals
Post-Entry Level – behaviors consistent with an autonomous practitioner beyond entry level
Program-Specific Expectations for Professional Behavior
Being a learner in the Program in Physical Therapy implies that you have made a commitment to the intensive and exciting training period that is required. The responsibilities connected with that commitment are many, just as they are numerous for the faculty. The following expectations for professional behavior are needed to meet these obligations. If a learner demonstrates unprofessional behaviors, faculty may use the Professionalism Concern Form to document and counsel the learner. Please refer to form at the end of the section on professional behavior.
The WashU Medicine Program in Physical Therapy team will promote a climate of mutual respect in the workplace.
I recognize and value differences as well as similarities in everyone by doing the following:
- Promoting a climate free of discriminating language and actions
- Encouraging open and honest communication
- Improving awareness of my own biases and beliefs and using that knowledge to improve understanding and acceptance
Examples include the following:
- Showing empathy
- Assuming good intent on the part of others
- Affirming others’ contributions
I value the work of others and their roles by doing the following:
- Behaving in ways that show respect toward others
- Developing relationships built on trust
- Promoting a climate that is equitable, inclusive, fair, supportive and responsive
- Creating a welcoming environment through words, actions and physical surroundings
Examples include the following:
- Greeting people in a pleasant way
- Looking for ways to help others, rather than focusing on how busy I may be
- Finding solutions to problems rather than complaining about them and/or blaming others
I empower myself and others by doing the following:
- Creating an environment where development of talent and ideas is encouraged
- Giving individuals the responsibility, freedom and resources to fulfill their roles
- Supporting opportunities for others to grow professionally
- Taking pride in my work
Examples include the following:
- Remembering that everyone is human, errors are inevitable, and that errors should be treated as opportunities to improve, rather than communicating shame or guilt
- Sharing information about processes and tasks with other Program members and understanding that keeping the information to myself does not translate into job security
I encourage teamwork by doing the following:
- Accepting responsibility for establishing and maintaining healthy interpersonal relationships with each member of the Program
- Creating opportunities for people to work together to serve our visitors, patients and each other
- Encouraging open sharing and exchanging of information and ideas
- Understanding how our roles and individual expertise support the success of the entire Program
Examples include the following:
- Not engaging in bickering, backbiting, or blaming others
- Talking only to you in a prompt, respectful manner if I am having a problem with you
- Talking to a person’s supervisor about an issue only if I need advice or help in deciding how to communicate appropriately, or in the event that direct communication with the person is not possible or not effective
- Not complaining about other team members. If I hear others doing so, I will respectfully ask that they talk to that person and/or their supervisor directly
Demonstrate Professional Classroom Behavior
Come to class
Make the investment you are putting into your future career worthwhile- come to class. Your ultimate obligation to your patients implies an interest in learning the most you can. All faculty members expect learners to attend class.
Classroom discussion and lab participation will enhance your assigned readings. Attention during class will enhance your understanding of information, no matter what your learning style is. Class participation and clinical experience will form the basis for your developing sound clinical judgment. At times, attendance in class will be mandatory and attendance may be taken at any time. Absenteeism is a reflection of your reliability and an indication of your professional work habits in the future. Patterns of being absent will be considered when assessing your performance in the curriculum. Treat being a PT learner as your full-time job.
The faculty does understand there will be occasional absences. If you are absent, it is your responsibility to obtain course materials and class notes from your classmates and to meet with faculty to clarify questions.
Be prepared in advance for class
Being prepared for class saves time (an important commodity) because it allows you to direct your questions toward areas of true confusion rather than general lack of knowledge. You contribute to your classmates’ learning through your questions as they contribute to yours with their questions.
Be prompt
Come to class, clinical experiences, and meetings on time. It benefits you and is your professional responsibility. It is a courtesy to the faculty, your patients, and your classmates. Hand in assignments on time. Not only will that allow you to avoid penalties, which may affect your grades, it will help you to keep on time for other commitments.
Be courteous
Even in times of stress, be courteous to your classmates, staff, and all faculty members. All will appreciate your efforts and will certainly reciprocate. In recent years, class members have been increasingly upset with classmates who are not courteous. Discourteous behavior is not acceptable in the classroom under any circumstance.
Examples of discourteous class behaviors that are not acceptable include ringing cell phones, using text messaging or e- mail during class, wearing hats, sleeping, talking during lectures, interrupting lecturers excessively, being late to arrive or in returning from break, packing up early, and using non-verbal behaviors which would commonly be judged as impolite. Learners who are discourteous in class will be advised and may be asked to leave a class if their behavior continues to be a problem. Repeated infractions will be reported at PT CAC as a deficiency in professional behavior.
Help to keep the space neat, clean and professional looking
Learners are responsible for putting away all equipment and supplies used during class each day. Learners are responsible for resetting the classroom furniture each day. Learners must be sure not to leave trash, food containers, food, or dishware behind in any of the space. Items left behind will be discarded weekly. Faculty members are responsible for keeping the stage and podium neat and professional looking. Faculty and learners will need to follow cleaning procedures following each lab and the Housekeeping department will provide additional cleaning of the space in the evenings. Any problems with the space or supplies should be reported immediately to staff.
WashU Medicine Program in Physical Therapy Professionalism Concern Form
It is essential that every learner in the Program in Physical Therapy understand the processes by which standing in the program is determined and the mechanisms which guide promotion and graduation decisions. It is also important that learners understand their right to appeal any decision and the steps necessary to accomplish appeal. This section of the learner handbook discusses those areas of the Program policies and procedures.
A learner must not receive or provide any unauthorized assistance on an examination. During an examination, a learner may use only materials authorized by the faculty.
In taking all written and practical exams, learners have the responsibility for preventing and reporting all occurrences of dishonesty. All exams must be completed independently by each learner. To prevent dishonesty all learners must protect the privacy of their own and other learners’ exams and papers.
During and after any written exam there will be no discussion about the exam in the presence or hearing of anyone who has not completed it, whether you are on or off the premises.
During and after assessments, there will be no discussion about the assessment with any learner, whether or not they have taken the exam. This includes discussion during the return of graded exams. The reason for this strict rule is that if a learner has not passed an assessment, a different case will be used on the make-up exam. Discussion among learners may unwittingly expose learners to cases they may encounter on a future exam. Fair re-examination can only be offered when learners have not been privy to prior discussion about the case.
In all academic work, the ideas and contributions of others must be appropriately acknowledged and work that is presented as original must be, in fact, original. Using an AI-content generator (such as ChatGPT) to complete coursework without proper attribution or authorization is a form of academic dishonesty. If you are unsure about whether something may be plagiarism or academic dishonesty, please contact your instructor to discuss the issue. Faculty, learners and administrative staff all share the responsibility of ensuring the honesty and fairness of the intellectual environment at WashU Medicine.
All learners and faculty are responsible for reporting violations or the appearance of violations of these rules to the course coordinator or another faculty member. In accordance with program policies on due process, any learner found to have violated the rules will be penalized.
Attendance and Participation
The goal of the physical therapy program is to graduate competent diagnosticians and highly skilled and safe practitioners of physical therapy. Therefore, learners are expected to attend all classes, prepare for all classes and actively participate in laboratory sessions and class discussions. Failure to do so may jeopardize your ability to reach this goal. Learners are also expected to report all anticipated absences to the module lead in advance of the class and determine what is necessary to make-up the class time missed. All learners are responsible for obtaining class materials from another classmate, unless special arrangements are made in advance with the faculty member. Repeated unexcused absences may result in disciplinary action by the PT CAC.
Command of previous material
As this is a professional program, you are always responsible for material covered in pre-requisite or previous PT courses. This includes basic scientific background, screening information, skills needed for patient assessment and treatment, and professional behavior. If you find you have deficiencies in these areas, you may consult the faculty for how to enhance your knowledge and skills.
Minimum passing standard
Our commitment to high quality performance in our program and to eventual competence in the clinic has resulted in our electing a general standard of acceptable performance of 70% or above in competencies and keywords. Both performance and written assessment data, described below, will be combined to determine whether learners pass both by competency and keyword. Competencies and keywords assessed through a rubric will have elements that will be transparent to learners prior to the assessments.
WashU PT Keywords
Anatomy, Cardiovascular Conditions, Exercise Physiology, General Medical Conditions, Kinesiology, Musculoskeletal Conditions, Neuroscience, Physiology, Pulmonary Conditions.
Grading Criteria
All courses in the curriculum use a pass/fail grading criterion. The curriculum contains curricular module, domain and clinical education courses. For each course a determination of pass/no pass will be made based on the full completion of required course elements and achievement of the appropriate course objectives and curricular milestones as determined by the PT CAC. End-of-course “pass/no pass” determinations will be made by the PT CAC at the end of each Phase.
The clinical education course criteria are set by the Clinical Education Team with consultation from other faculty. Criteria for successful completion are listed in the course syllabi for these courses.
Failure to meet the minimum passing standard and course expectations will result in review at PT CAC.
Grade point average (GPA) is not calculated for the pass/fail courses. However, the Program recognizes that some external entities require learners to submit a GPA metric as part of their application processes, for example, in Residency applications or auto insurance applications. The Program may provide a GPA calculation upon request by a learner to be submitted to these external entities. To reiterate, any GPA calculation requested for an external entity is not used by the Program internally for progression-related decisions.
When learners do not meet the standards for each course, promotion may not occur. At any time, if a learner is on a trajectory towards failure to attain competence in any domain or keyword, it is the learner’s responsibility to contact the appropriate faculty member to discuss actions or required remediation.
Assessment of Competence
Assessments will be spaced throughout each module and each assessment event will contribute to measurement of competence in differing ways. Each assessment event will also be labeled by assessment type. The assessment type is determined by how the assessment contributes to competence. Required learning activities are considered an instructional method and are organized within the learning management system by Module Course. Required learning activities will contribute to competence via their timely completion and contribute to the Professionalism Domain. Assessment for and of learning contribute to competence and are organized within the learning management system by domain course. Assessments of learning, or summative assessments, are assessments that occur at critical points across each phase, and may or may not have a passing standard. For assessments of learning that have a passing standard, if a learner does not pass an assessment of learning on the first attempt, a learner will be provided a second attempt. If the learner does not pass the second attempt, the learner will be referred to the PT CAC. Performance assessments for learning, or formative assessments, occur frequently and have no passing standard. Each learner is encouraged to repeat performance assessments for learning to guide their ongoing learning and performance improvement. Learners will not have the ability to repeat written assessments for learning.
There are two primary methods by which learners are assessed for competence, by performance assessments and written assessments. Below is the general description of each assessment method and type as it contributes to overall assessment of learner competence.
Performance Assessments
Assessment data will be available in the Competency.AITM database. Assessments of learning must be passed by achieving the passing standard on the event as determined by faculty. Please see above (Assessment of Competence) for procedures when an assessment of learning is not passed. To be eligible to sit for the of learning assessment, all required learning activities must have been completed and submitted.
Practical examinations
Assessment data will be available in the Competency.AITM database. Assessments of learning must be passed by achieving the passing standard on the event as determined by faculty. Please see above (Assessment of Competence) for procedures when an assessment of learning is not passed. To be eligible to sit for the of learning assessment, all required learning activities must have been completed and submitted.
Assessment for Learning
Assessments for learning occur frequently and are meant to inform ongoing learning and improvement. Any reassessment for improvement will never penalize a learner. The best performance on each item within the assessment event will be used as the competency contributing assessment. Protected time has been allotted within scheduled class for reassessment. In rare circumstances, module leads may schedule additional class hours for reassessment. Learners should view all re-assessment as an opportunity to receive feedback for growth and improvement.
Assignments
Assessment data for assignments will be available in the Competency.AITM database. Summative assignments with a passing standard must be passed by achieving the passing standard on the event as determined by faculty. Summative assignments that do not have a passing standard will have one submission and learners will not have an opportunity to resubmit the assignment.
Learners are expected to follow the directions on all assignments. Assignments may be intended as either individual or group work. If an assignment is to be done by an individual learner, it is expected that all learners will produce original work independently. If an assignment is to be completed in groups, all learners in the group are expected to participate equally and the work must be completed by the members of that group only. Further, any performance improvement assessments for group work must be completed by all group members. Learners may not use papers written by previous learners to prepare their own papers. Learners must turn in papers when and where they are due. If learners do not turn in assignments by the due date and time, this will be reflected on assessment within the Professionalism domain and may result in referral to PTCAC. Each learner has the responsibility for reporting to the faculty member any actions in violations of the above policies.
Written Assessments
Learners will complete all written assessments within Exam Soft. Written assessments for learning will aggregate by both competency and keyword over the Phase. Each written assessment for learning will have a practice assessment within Exam Soft. These practice assessments are required learning activities and will contribute to competence via their timely completion and contribute to the Professionalism Domain.
Assessment Appeals
Learners must approach the module leads, or the Director of Clinical Education if the appeal is related to Clinical Education, to discuss or appeal a score on any assessments within one week (5 working days) after the results are posted.
Assessment Return and Review
The primary means for reviewing assessment data is through Exam Soft and Competency.AITM. Faculty will perform written and performance assessment review and results will be available within Competency.AI. Written assessment review within Exam Soft will occur during performance improvement scheduled class time scheduled after written assessment completion. Extenuating circumstances or excessive time needed to hand-grade assessments may increase the time it takes to get assessment results back to learners.
During and after any written exam there will be no discussion about the exam in the presence or hearing of anyone who has not completed it, whether you are on or off the premises. Any learner caught reproducing any part of an exam or discussing the exam with others who have not yet completed the exam will be referred to PT CAC for faculty discussion of their academic misconduct.
During and after performance exams, there will be no discussion about the performance exam with any learner, whether or not they have taken the exam. This includes discussion during the return of graded exams. The reason for this strict rule is that if a learner has not passed a performance exam, a different case will be used on the remediation exam. Discussion among learners may unwittingly expose learners to cases they may encounter on a future exam. Fair re-examination can only be offered when learners have not been privy to prior discussion about the case.
All learners and faculty are responsible for reporting violations or the appearance of violations of these rules to the course coordinator or another faculty member. In accordance with program policies on due process, any learner found to have violated the rules will be brought forward to PT CAC.
If the expectations for individual or group work are violated, the actions of the learner(s) will be reported to PT CAC for consideration of academic misconduct. Learners who are uncertain as to what constitutes academic dishonesty, including plagiarism, are referred to the WashU Medicine website under academic policies https://wustl.edu/about/compliance-policies/students/
Course Failure and Appeal
Please refer to PT CAC policies and procedures in this handbook.
Exam Policies
Arriving late to an exam is not consistent with professional behavior and disrupts the faculty member and all learners. The following policies are in place to provide a professional environment. All learners must be physically present in the assigned testing room and may not take any written examination remotely.
Arriving Late to Exams
Learners must arrive on time to all exams or quizzes. Late arrival is defined as immediately after the posted start time. Written exams must be downloaded within Examplify prior to the start of each exam. Failure to do so may result in an inability to sit for the exam at the scheduled time.
A learner arriving late to a performance assessment where a lab assistant serves as the “patient” or subject will be allowed to begin the exam but will not be given more time than remains for the test. Late arrivals may also result in a deduction from the assessment grade in the professionalism domain.
Missed Exams
Learners must contact the module lead in advance if they anticipate they will be missing an exam (e.g. due to illness or family emergency). A learner who misses an exam due to a valid and excusable reason, as determined by the module lead must contact the appropriate module lead to schedule a date and time for the make-up exam.
If the module lead observes repeated lateness on the part of a learner, she or he will bring the issue of unprofessional behavior to the attention of PT-CAC for action.
Performance Assessment Rubric
Performance assessments will be evaluated with a rubric. Below is the rubric template that will be used throughout the curriculum. On each rubric, elements will be provided to allow students to prepare for upcoming assessments. Additional elements are items where a learner may receive formative feedback to drive their learning, but are not required. Learners will have a clear understanding of the elements and performance expectations prior to all assessment events.
Assessment Feedback
What is the most important thing that the learner is doing well that should be continued?
What is the most important thing learner can improve on before the next assessment?
| Items | Significant Concern | Needs Improvement | Meets Expectations | Exceeds Expectations | Item Feedback |
| Item: Elements: Additional elements for formative feedback | Description of significant concern | Description of needs improvement | Description of meets expectations | Description of exceeding expectations |
At the outset of the Doctor of Physical Therapy (DPT) Program, learners should be informed about the program’s educational and performance standards and expectations. This document serves to organize the policies and procedures by which decisions of competency attainment are made and communicated. The policies and procedures listed below are adopted by the faculty and administration of the Program in Physical Therapy concerning the determination of learner attainment of competency and is communicated to all relevant stakeholders.
Overall academic and professional evaluation of Doctor of Physical Therapy learners in the Program in Physical Therapy DPT Curriculum (hereinafter “DPT Curriculum”) at WashU Medicine (hereinafter “WashU Medicine”) will be made by the Competency Attainment Committee (hereinafter “PT CAC” or “Committee”).
Preface
This document describes procedures adopted by the faculty and administration of the Program in Physical Therapy concerning review of student attainment of competency. Students are encouraged to read this information for a thorough understanding of the content.
Major revisions to this document will be approved by the Faculty of the Program in Physical Therapy.
Questions about this document may be directed to:
- Director of the Program in Physical Therapy
- Division Director of Education
- Assistant Director of Student Assessment and Program Evaluation
I. Students for Whom the Rules Apply
A. The rules governing operation of the Competency Attainment Committee (PT
CAC) apply to students in the following categories:
- Students engaged in any phase of the DPT Curriculum
II. Competency Attainment Committee (PT CAC)
A. Purpose and Jurisdiction
- In order to successfully complete their studies in the Program in Physical Therapy, students must demonstrate the ability to become a safe and effective physical therapist by the attainment of competency in the eight competency domains identified by the program:
i. Patient and Client Care
ii. Knowledge for Practice
iii. Practice-Based Learning and Improvement
iv. Interpersonal Communication
v. Professionalism
vi. Systems-Based Practice
vii. Interprofessional Collaboration
viii. Personal and Professional Development - Progress toward and attainment of competency within these domains and their associated competencies and the keywords will be determined by the Competency Attainment Committee (PT CAC).
- Throughout the enrollment of a student, it is within the jurisdiction of the PT CAC to terminate the enrollment of a student who has failed to attain competency in any of the domains. The principle that careful selection of students for admission will minimize attrition from the program is strongly endorsed by the PT CAC.
- The text contained herein outlines rules governing the review of student performance.
B. Responsibilities of the Competency Attainment Committee
Review of the evidence supporting progression toward and attainment of competency of students in the Program in Physical Therapy will be made by the PT CAC. The deliberations of the PT CAC are generally positive in approach and are committed to the ultimate aim of assisting students in successful completion of the DPT curriculum through the attainment of competency in all eight domains.
The PT CAC has several important roles including, but not limited to, the following:
- Review of all assessment data, via individual student competency portfolios, to determine if a student has, or is on a trajectory to, attain competency in each domain and keyword.
- Make decisions regarding a student’s academic progress, including the following:
- Promotion to the next phase of the curriculum.
- Remediation, with or without promotion, for any student who has not yet attained competency in a particular domain or keyword.
- Probation, Suspension, or Dismissal or other measures to address lack of satisfactory academic progress. Review of any remediation processes to determine if competency has been attained following remediation efforts.
- Approve any leave of absence greater than one year, owing to the impact on competency attainment as competence is a longitudinal process.
- Determine those students who have successfully completed all prescribed requirements of the Program and are qualified to receive the Doctor of Physical Therapy degree.
C. Appointed and ex officio membership:
- There will be a minimum of 10 voting members of the PT CAC representing the eight domains of competence as well as the curricular modules under evaluation.
- In addition, PT CAC membership may include voting ex-officio members based on their positions within WUSM or the PT Program as well as their broad understanding of the competency-based program of assessment. These ex-officio members may include the Division Director of Education, Associate Director of Professional Curriculum, Director of Clinical Education, and Assistant Director of Student Assessment and Program Evaluation. The Division Director of Education will serve as the PT CAC Chair and will only vote in the event of a tie among the voting members present. A representative of the Medical School faculty appointed by the Dean of the School of Medicine will serve as non-voting Co-Chair. The Director of the Program in Physical Therapy, the Assistant Director of Diversity, Equity and Inclusion for the Program in Physical Therapy, and the Director of Student Health Services may also attend the PT CAC meetings as non-voting, ex officio members. Family members of a student and any member of the committee who has participated in the clinical care of a student must recuse themselves from any deliberation regarding competency attainment.
- Guests: Any faculty, administrator, student or staff member may be invited as a guest at the discretion of the PT CAC Chair if their presence is deemed important in making decisions of competency attainment. Any invited guest may be asked to provide additional information prior to, during or after the meeting.
D. Meeting Frequency and Quorum
- PT CAC meetings occur throughout each phase of the DPT Curriculum with sufficient frequency to:
- Allow for review of assessment data to determine if a student is on trajectory to achieve competence in each Domain and keyword.
- Allow reasonable opportunities for early support and remediation to be completed, if required. In these circumstances, students will be notified of ad hoc competency review by the PT CAC.
- Make decisions near the completion of each phase regarding promotion, remediation with or without promotion, probation, or dismissal.
- PT CAC meetings may be called ad hoc when egregious concerns regarding competence occur.
- Quorum will constitute attendance, virtual or in person, of (3/4) of the voting members. A simple majority vote of the members present shall be required for all decisions, except decisions to dismiss a student for academic deficiencies and decisions to recommend that a student be suspended or expelled for academic or professional misconduct, which requires a three-quarters (3/4) majority vote of the members present.
E. Deliberations and Outcomes
- Competency Attainment Committee (PT CAC) deliberations and outcomes will be summarized in the meeting minutes. Students will be notified in writing by The Chair of PT CAC of all decisions generally within 14 days of the decision.
- Decisions regarding dismissal will be reported to the DPT Program Leadership and other stakeholders, as needed. Decisions of remediation without progression, dismissal, probation, will also be communicated to Financial Aid to support necessary alterations in aid.
F. Conflicts of Interest
- Situations may exist in which a PT CAC member has a conflict of interest such that the PT CAC member is unable to objectively perform their duties and evaluate a particular student. In such a case, the PT CAC member must recuse themselves from participation in deliberations and decisions regarding that student.
III. Achievement of Standard and Competency Attainment
- Academic Credit
- The curriculum contains curricular module, domain and clinical education courses. For each course a determination of pass/no pass will be made based on the full completion of required course elements and achievement of the appropriate milestone as determined by the PT CAC. “In-progress” will be recorded on the transcript until such time as a student has completed all required elements. End-of-course “pass/no pass” determinations will be made by the PT CAC at the end of each Phase.
- Competency Attainment
- Decisions of competency attainment will be made by the PT CAC based on the totality and sufficiency of evidence regarding a student’s performance in each of the domains of competence and keywords. The evidence required for determination of competence has been determined by the PT CAC, in conjunction with the Program faculty. Decisions of competency attainment will be recorded on the transcript at the completion of each phase of the curriculum. Student progression towards successful competency attainment must occur at the midpoint of each academic year in order for financial aid to disperse funds to students. The PT CAC will meet at the appropriate times to make such determinations.
- Remediation
- When a student has not demonstrated competency or is on trajectory towards failure to attain competence in any domain or keyword, the PT CAC will recommend that student for academic support. In some instances, a student’s trajectory can be addressed through informal means such as discussion with their coach. Formal remediation decisions will be determined by the PT CAC with supportive evidence from assessment.
- Dismissal, Probation, and Other Remedial Measures
- When warranted, such as in situations including but not limited to persistence of dyscompetence despite remediation or marked critical deficiency, the PT CAC may decide a student warrants dismissal, probation, or other remedial measures. While the PT CAC encourages the use of progressive actions and opportunities for remediation, the nature or severity of the dyscompetence may prompt, at their discretion, more immediate or severe actions.
IV. Misconduct
- Student misconduct is governed by the University Student Conduct Code. Allegations of student misconduct which may constitute an offense under the University Student Conduct Code will be handled in accordance with the provisions of that Code. The University’s Director of the Office of Student Conduct and Community Standards receives and investigates alleged violations of most forms of misconduct under the Code, with Academic and Professional Misconduct being a notable exception, as described in Section IV.B, below. See University Student Conduct Code (http://www.wustl.edu/policies/judicial.html) for a full discussion of the University Student Conduct Code.
- Academic and Professional Misconduct are special forms of misconduct under the University Student Conduct Code. The University Student Conduct Code provides that PT CAC may hear and decide cases of alleged Academic and Professional Misconduct. PT CAC shall handle such allegations using the following procedures:
- Academic or Professional misconduct shall include, but is not limited to: breaches of personal confidence and trust, including cheating, unauthorized use of materials during examinations, or other academic misconduct; abuse, misrepresentations or other seriously improper conduct in relation to patients or colleagues including breaches of confidentiality; illegality; substance abuse; failure of judgment including that related to non-compliance in the treatment of any personal medical condition; other misconduct in violation of University policy or the University Student Conduct Code, or the APTA Code of Ethics; and misrepresentation or failure in personal actions or in meeting obligations, so as to raise serious unresolved doubts about the integrity of the student.
- Procedures for Review
- Matters involving possible breaches of the University Student Conduct Code by DPT students shall be brought to the attention of the PT CAC Chair. The individual(s) raising the questions of possible misconduct shall present them to the PT CAC Chair in writing and provide other detailed written information as necessary. Individuals submitting information are reminded of the need for confidentiality regarding all matters of potential misconduct.
- The PT CAC Chair shall determine, in consultation with the Co-Chair of PT CAC, whether the alleged conduct, if true, could constitute misconduct under the University Student Conduct Code. If the PT CAC Chair determines that the alleged misconduct could constitute Academic or Professional Misconduct, then PT CAC may retain jurisdiction to consider the alleged misconduct pursuant to the procedures described in this Section IV.B. The PT CAC Chair also has the discretion to refer the matter to the University’s Office of Student Conduct and Community Standards or other applicable University office, based upon the nature of the allegation. For example, a complaint alleging that a student has committed a sexual assault would be handled by the Gender Equity and Title IX Office.
- If the PT CAC Chair deems it appropriate upon review of the alleged Academic or Professional misconduct, they will convene a meeting of the PT CAC. The student shall be notified of this meeting. The PT CAC shall, whenever possible, convene within two weeks after the initial meeting between the student and the PT CAC Chair (or designee). Should a student be referred to the PT CAC for an issue(s) involving both standard and competency attainment performance and academic or professional misconduct, the procedures regarding academic or professional misconduct will be followed.
- The Committee is not positioned in an adversarial role against the student but serves to review the evidence as presented and render its decision regarding disciplinary action if necessary. The PT CAC will consider evidence which tends to prove or disprove the alleged conduct. If the PT CAC finds that the student engaged in misconduct, it may consider additional evidence of prior conduct, evidence as to the charged student’s character, the student’s academic record, or any other evidence which could assist the PT CAC in determining an appropriate sanction. The PT CAC Chair will rule on whether or not specific evidence or testimony will be considered. The PT CAC has neither the advantages nor limitations inherent in a court of law. During the meeting the student will have access to the evidence presented and may present evidence on his or her behalf, subject to reasonable limitations as to amount, scope, and format, as determined by the PT CAC Chair.
- The decision as to whether the student committed the alleged misconduct will be made solely on the basis of evidence and testimony presented at the meeting. Innocence of the student will be presumed. A PT CAC member must find in favor of the student unless the member is persuaded that it is more likely than not that the student engaged in the misconduct alleged.
- If the person who has submitted the charges of misconduct is a member of the PT CAC, that member will provide information about the professionalism issue to the PT CAC but will then recuse him/herself from deliberation and voting.
- The written record of such proceedings will be held confidentially with access restricted to Committee members, the student involved, and members of the Program or WU Administration involved in the proceedings.
- Unless it is determined by the PT CAC Chair that extraordinary circumstances exist, the student will be permitted during the PT CAC proceedings to attend class (but not clinical activities) so long as the student does not pose a threat to himself/herself or others
- Possible Sanctions for Academic or Professional Misconduct
Any Committee decision regarding a complaint of alleged academic or professional misconduct will be communicated in writing to the student within a reasonable time after the Committee meeting, generally within ten business days of the Committee meeting.- Warning or Probation, and other Sanctions
A student shall be given a warning and may be placed on probation by the Committee upon a finding that he/she has engaged in Academic or Professional Misconduct. The Committee may also impose other sanctions, including requiring some form of educational remedy and evidence of readiness to function in a professional manner to remove a probationary status. Students placed on probation may be asked to resign from holding a class office or other leadership positions. - Suspension or Expulsion
In cases where a student has exhibited significant or repeated Academic or Professional Misconduct, the Committee may decide to suspend or expel the student.
- Warning or Probation, and other Sanctions
V. Reconsideration and Appeals Procedures
- If competency attainment cannot be achieved, or misconduct has been determined as described in Section IV.B above, the PT CAC may render a determination of remediation with promotion, remediation without promotion, probation, dismissal, suspension, expulsion, or other sanctions. A student may request a reconsideration or appeal decisions made by the PT CAC as described below.
- Reconsideration: Decisions of remediation with promotion and probation are not available for reconsideration and are based on the expert judgment of the PT CAC. A student may request that PT CAC reconsider remediation without promotion, academic suspension or dismissal or decisions regarding Academic or Professional Misconduct. Note: actions taken by entities other than the PT CAC (e.g., the Dean or the University Student Conduct Board) are not subject to requests for reconsideration or appeal under this Section V. A written request and rationale for reconsideration must be received by the Director of the Program within ten (10) calendar days of the date of the PT CAC decision. Such a request for reconsideration should be based solely on (i) the need for PT CAC to consider additional information which was not previously presented to PT CAC for good cause; and/or (ii) a contention that pertinent PT CAC procedures were not followed during the original proceeding such that the decision is unfair. The decision to grant a Request for Reconsideration is within the sole discretion of the Director. If the Director decides to have PT CAC reconsider its decision, the Director shall notify the student in writing of the decision to reconsider and shall advise PT CAC to reconvene within thirty (30) days of receipt of the written request to reconsider. During the reconsideration process, the student will be permitted to attend class (but not clinical activities) so long as the student does not pose a threat to themselves or others. The Committee may reverse, modify or affirm its original decision based upon its reconsideration and/or input from the student or others.
- Appeal Procedures
Only one type of decision by PT CAC is appealable to the Dean of WashU Medicine with respect to academic performance and competency attainment decisions. A student may appeal to the Dean following a dismissal for standard and competency attainment deficiencies. The decision of PT CAC to impose a warning, probation, or any academic action other than dismissal for academic performance deficiencies is final and not appealable.
In cases involving academic or professional misconduct and a finding of responsibility against the student, the student may submit an appeal as set forth below.- Any such appeal described in this Section V.C. above, must be made in writing to the Dean within fourteen (14) calendar days after the student receives the final written decision of PT CAC (either the initial decision, or a decision denying a timely request for reconsideration, or a decision after reconsideration, if granted). Students are not required to request reconsideration by the Committee prior to appealing to the Dean; however, if reconsideration is requested, appeal to the Dean should not be made until the Director has ruled on the reconsideration request.
- The scope of the appeal must be limited to the grounds that a fair hearing was not provided, or that the action taken was excessive. Such written appeal must clearly state the grounds for the appeal and must include all supporting information which the student desires to be considered as part of the appeal.
- When such appeal is taken, the Dean shall not substitute their judgment of the facts for that of the PT CAC. In deciding the appeal, the Dean may utilize, at their discretion, an ad hoc appeals committee to advise them on the merits of the appeal. Members of the appeal committee must be faculty members at WashU Medicine. Members of PT CAC are not permitted to participate on an appeals committee for decisions on which they voted.
- The Dean shall have thirty (30) days from the date of receipt of the appeal to decide the appeal, unless extended by the Dean upon notice to the student, and the decision of the Dean shall be final. The Dean may decide to uphold the decision of PT CAC, reverse the decision of PT CAC, or remand the matter to PT CAC with instructions for additional proceedings. The Dean’s decision will be communicated in writing to the student and to PT CAC.
Maintaining academic integrity is a responsibility for all students and faculty. Without it, we fail to preserve the rights and safety of our patients and fellow professionals, and we fail to meet the expectations of our profession.
Offenses of academic integrity include any action that violates the Judicial Code of the university as reported in University Student Conduct Code, the document of policies and procedures at WashU. https://wustl.edu/about/compliance-policies/academic-policies/university-student-judicial-code/
One offense of academic integrity is academic misconduct, defined in the Judicial Code:
Academic or professional misconduct, including, but not limited to, cheating, plagiarism, fabrication of data or records, impermissible collaboration on assignments, misrepresentation of student status or identity, resume or credential falsification, unauthorized use of prescription medication to enhance academic performance, unauthorized use of electronic resources, violation of test-taking conditions or rules, or otherwise violating the applicable Academic and/or Professional Integrity Policy. Knowingly making false allegations of academic misconduct against any student will itself be considered a form of academic misconduct.
Academic misconduct also violates the APTA Code of Ethics. Below are guidelines for reporting incidents of academic misconduct. Students and faculty observing other students engaging in activity that is academically dishonest share the responsibility that the incident is dealt with appropriately and in a timely fashion.
- Student observes academic misconduct
- If a student chooses to take action at the time of the occurrence (e.g. during a test) the student shall
- inform the course coordinator about the observed behavior
- document the observed behavior after the incident and give it to the course coordinator
- If a student chooses to take action after the time of the occurrence (e.g. after a test) the student shall
- confront the other student using appropriate communication skills to obtain that student’s account of the incident inform the alleged student that the incident will be reported to faculty because of University and Program policy report the incident to the course coordinator or other faculty member
- document the incident in writing for faculty action (see below for the guidelines faculty follow based on the willingness of students to document academic misconduct.)
- If a student chooses to take action at the time of the occurrence (e.g. during a test) the student shall
- Faculty member observes academic misconduct with or without student corroboration:
- If a faculty member chooses to take action at the time of the occurrence (e.g. during a test) he or she shall
- inform the student about the observed behavior
- obtain the student’s account of the situation report the incident to the Associate Director for Professional Curriculum or the Education Division Director
- follow the policy of PT CAC
- If action is delayed until after the time of the occurrence (e.g. after a test) the faculty member shall
- confront the student and obtain the student’s account of the situation
- report the incident to the Associate Director for Professional Curriculum or the Education Division Director
- follow the policy of PT CAC
- If a faculty member chooses to take action at the time of the occurrence (e.g. during a test) he or she shall
- Faculty member receives a student’s report of academic misconduct of another student but did not observe the incident directly
- Confront the student reported to be dishonest and share that a report was made to you; then obtain the student’s account of the incident
- Ask students who report incidents to you to document their observations for PT CAC and encourage them to confront their peers; inform them that without their documentation of the incident you cannot take definitive action except to counsel the alleged student; only with their documentation can the matter be acted upon
- Assess the situation
- If you agree that academic misconduct has occurred
- Document the incident and discussions with the student
- Report the incident and your proposed action to the Associate Director for Professional Curriculum or the Education Division Director
- if you are comfortable with the action to take, proceed and then report what your actions were to the Associate Director for Professional Curriculum
- if you are uncertain about what actions to take, report the incident to the Associate Director for Professional Curriculum for a decision
- If you cannot ascertain if academic misconduct has occurred and the reporting student is willing to document the incident
- report the incident to the Associate Director for Professional Curriculum or the Education Division Director
- If you cannot ascertain if academic misconduct has occurred and the reporting student is unwilling to document the incident
- document the incident and submit the report to the Associate Director for Professional Curriculum who will then submit it to the Coordinator of Admissions and Student Affairs for the student’s record
- If you agree that academic misconduct has occurred
Students who report incidents of academic misconduct will be referred to anonymously at PT CAC meetings, e.g. by referring to them as “student A” or student “B” etc. Students whom the faculty member believes have been academically dishonest, or students about whom fellow students are willing to submit documentation, will be referred to without a name during the initial discussion of the incident. PT CAC will be informed of the student’s name after agreement has been reached on the actions to take.
Any student not completing a semester or clinical experience that they are currently enrolled in may be eligible for tuition reimbursement per the timeline outlined in this policy. Not completing a semester or clinical experience may be for any of the following reasons: withdrawal, leave of absence, remediation that alters a student’s progression, suspension, or dismissal. Notice of not completing a semester or clinical experience must be submitted by the student to the Program in writing. Please see timeline below for refund schedule.
| Timepoint | Refund |
| Stops attending prior to first week | Tuition refunded in full |
| Stops attending prior to midpoint of semester or clinical experience* | Tuition refunded, prorated by week |
| Stops attending after midpoint of semester or clinical experience* | No refund |
*midpoint is determined by the number of weeks in the semester or clinical experience
Minimum system requirements for test-taking software are necessary for successful completion of the program. They can be accessed here: https://examsoft.com/resources/examplify-minimum-system-requirements/
Ordinarily, students must complete the academic program for the DPT degree within a maximum of three years, unless they have been permitted to extend this time frame upon admission or during the program.
Leave of Absence
Students who are unable to maintain continuous enrollment status must request an official Leave of Absence (LOA) from the program. The program follows the voluntary and involuntary LOA policies at the School of Medicine. Any LOA greater than 1 year or any additional LOAs, consecutive or otherwise, after a student has already taken a LOA are typically not allowed and would require additional approval through a request for extension from the PTCAC. More information can be found in Workday.
Recency of Credit
All work for the DPT must be completed within four years of the time of admission.
Request for Extension
A student approaching the four‐year maximum may be granted an extension. This extension may not exceed one year. The request for an extension must be made to the PTCAC and must include a reason the extension is necessary with a detailed time frame for completion of remaining work.
To accommodate student absences and for students who would like to review past course content, all large group class sessions will be recorded and made available for all students. All recordings are copyrighted and considered property of the Program. Students should not share them with others nor copy them in any manner. Please note that despite recordings being made available to students, the faculty still expects student attendance in class except in the case of illness or an excused absence (family emergency, critical illness in the family, funerals for immediate family, required court appointments, and medical appointments that cannot be scheduled except during class time).
Students may use personal equipment to audiotape or videotape any lecture only if advanced permission is obtained directly from the lecturer in advance of the lecture.
The Program follows copyright law. All members (faculty, staff, and students) of the Program in Physical Therapy are expected to comply with copyright law. Copyright law provides the legal right to authors of original works to protect the authors’ rights to obtain commercial benefit and to control how the work is used.
How are Program members expected to comply with Copyright Law. Faculty, staff and students are prohibited from providing multiple classroom copies of the following items unless the publisher of such material has given explicit permission for classroom distribution:
- published articles or portions of books
- figures, tables, text etc. that were obtained from copyrighted material
- copies of power point presentations that contain copyrighted material
Faculty, staff and students are allowed to print out or photocopy one copy of an article for their personal use.
No copyrighted material may be posted on course or Program web sites unless explicit permission from the publisher has been obtained. At times faculty members may have the library post material on e- reserve.
All course materials created by faculty, adjunct faculty, and students are protected by copyright law. All material distributed in print, via electronic media, or on the Internet by the Program in Physical Therapy is considered copyrighted material. Students are prohibited from copying materials for distribution without express permission of the author (e.g. professor) and giving credit to the originator of the material. Students may not sell any material or use it for commercial interests.
There are significant costs in obtaining copyright permission. Faculty will limit this at times to avoid passing on costs to students through fees or tuition increase.
For specific details of copyright law and WashU policy, please refer to the following website: http://www.wustl.edu/copyright/
Occasionally students will have the opportunity to co-author a poster presentation, oral presentation, or manuscript with faculty members. Students must seek counsel from the faculty regarding who is included as an author and in what order authors are listed. The university has careful guidelines on this practice, as do certain journals. Students will not be considered sole authors of any project done during their studies here.
- Faculty members shall notify the Director and the Division Director of Education at the time of submission of the abstract and when they have received notice of acceptance. Faculty member will then be notified is funding is available.
- A faculty member’s name and WashU Medicine Program in PT must be on the poster; if the presentation is a report on the student’s own work, the student’s name should be listed first.
- We highly encourage students to attend and present at the Missouri Physical Therapy Association state conference.
- We do not encourage students to miss class or clinical experience time to present posters or presentations, but will consider this an excused absence in the case of CSM or another physical therapy related conference. Students completing their clinical experiences must get permission to take time off from their clinical instructors.
- The Program will pay for the preparation of the poster, registration required of presenters at the APTA student member rate, and one night’s hotel stay. Any additional funds must be negotiated and are not guaranteed.
- If the work is a result of a final course and is submitted in time for the first possible opportunity to present at CSM or another physical therapy related conference following the student’s graduation from the Program (e.g. 2018 graduate presenting at 2019 CSM or June 2019 conference) the same level of funding will be offered to the recent graduate.
- Students will be encouraged to present their posters or other presentations to faculty for practice.
- When grant funds are available, investigators are free to handle funding for student presentations as they wish within the constraints of the funding agency’s policies.
- PhD students are not eligible for funding under this policy.
The University has very strict rules on the use of its logo on anything (clothing, stationery, signs, etc.). Please contact the DPT Admissions and Student Affairs Office to confirm whether your intention to use the University logo is acceptable.
Use of the Program in Physical Therapy name must meet acceptable standards of decorum. For example, some classes or teams have created their own t-shirts for special events or intramurals. Phrases, wording or drawings must be professional and inoffensive. Please note: The Program in Physical Therapy does not support activities where excessive drinking or risky behavior is encouraged. If such events are scheduled (e.g. pub-crawl), students may not place the University Program in Physical Therapy name on the t-shirt. Remember anytime you are wearing apparel with our name on it, you represent the Program. We expect that representation to be professional.
The University owns the computer equipment and software provided in the study rooms, lounge, breakout rooms and the first floor classroom. The equipment is maintained by WashU IT staff. Use of the equipment is restricted to students from the Program in Physical Therapy. The computers are provided primarily to facilitate completion of course-related work by students.
Please help us insure the greatest possible benefit to all students by adhering strictly to the following guidelines.
- Report all virus infections immediately to ithelp@wustl.edu (314-933-3333).
- Report all operational problems, such as, equipment malfunction, and software malfunction to WashU IT.
- Do not install or download any software, including games onto student computers.
- Do not alter any operating system settings including display, memory, communication parameters, printer drivers or any other environment settings.
- Do not alter any of the system files (e.g., config.sys, autoexec.bat, any .sys or .dll file).
- Do not alter any printer, network, mouse, keyboard, or monitor connections.
- Do not delete any files that you did not create.
- Do not store on the hard disks any files that you have created with the expectation that the files will be retained. The hard disks will be reformatted periodically, and the Program will accept no responsibility for lost user files. Each student will have access to file in the cloud storage (i.e. Box).
- The highest priority for use of the computers is course-related work. Thus, students using the computers for other purposes should yield to those who need to do course-related work. All users should be considerate of all other users in sharing the computers, especially during periods of heavy use (i.e., between classes).
- Printers should be used for course-related work only. System administrators will monitor the content and number of pages printed by each student.
- All users are responsible for refilling copiers with paper, clearing the work area of clutter before leaving the room, and keeping fluids away from the computers. Contact the receptionist at the front desk of the Program suite for copier problems.
Failure to comply with the User Guidelines will result in termination of computer user privileges for the offender and may result in removal of all student computers
Audiovisual equipment in rooms 2700, SSD Conference Room, 6700, 6701 and 1235 is available for use during class time only. Only trained work study students or Program staff and faculty members may operate the equipment. The computers at the podia in each classroom may not be used by students for personal use or studying. Anyone caught using the equipment will be reported to PT CAC for breach of professional conduct. Students may not use the equipment for any social events unless approved by the Director of the Program. Audiovisual equipment may not be taken outside of the Program. All malfunctions must be reported to the receptionist in the main office (room 1101 or PT-Technology@email.wustl.edu) immediately so appropriate repairs can be made. See also the policies on video/digital taping.
Students of the University who are not enrolled in the Program and wish to attend (audit or take) classes in our curricula must seek the approval from the Division Director of Education.
The DPT Student Handbook is a resource that addresses many issues related to all levels of students in the Program. The handbook is posted on the program website and is a resource specifically for professional students that includes helpful information about Program personnel as well as curriculum and matriculation policies.
To protect the confidentiality of students, faculty must request access to student academic records through the Program’s Office of Admissions and Student Affairs Manager. Academic records may not be copied or removed from this office. Students may access their own record only with written permission from the Program Director or the Division Director of Education.
Course files for all professional courses must be kept current in accordance with requirements of the Commission on Accreditation of Physical Therapy Education. It is a Program expectation that files for courses in other curricula be constructed in the same format as those for the professional curriculum. All course files are maintained by the Program Coordinator- Admissions and Student Affairs and kept electronically in Box. Contents of an electronic course file should include a current syllabus, all handouts for the current year, all exams for the current year, all syllabi and exams for the previous nine years. This assures access to contents during a full 10-year accreditation cycle.
Retention of Records
Individual responses for tests and quizzes graded in Canvas or ExamSoft and assessments graded in Competency.AI should be kept until the student graduates. The records of former students will remain confidential.
Faculty must have a written request from a student or a graduate before providing an employment recommendation. Forms to facilitate requests for references are available in the Student Commons course in the Canvas learning management system, but a written request in another format (e.g. e-mail or letter) also is acceptable. These requests should be retained by the faculty member.
The policies and guidelines here at WashU, WashU Medicine, and the Program in Physical Therapy relate to our educational mission. These policies, procedures and guidelines exist to assist WashU students, faculty and administrators with doing the business of WashU in ways that are effective, consistent and compliant and to provide a safe, effective and supportive environment in which to learn, teach and work.
Links to policies and resources are listed here. Some direct links are provided for specific policies. However, students are responsible for reviewing and complying with all relevant policies at the University, School, and Program. Students with questions about any policy should contact the Division Director of Education or the Associate Director of Professional Curriculum.
A complete list of policies for all students at WashU Medicine is here: https://bulletin.wustl.edu/medicine/policies/
WashU Medicine is committed to providing a safe, professional and supportive environment in which to learn. These policies and guidelines pertain to professionalism, appropriate conduct and student rights. They exist to protect students and employees as they conduct their daily responsibilities.
Included in the Policies and Guidelines of U Medicine are:
Demonstrations and Disruption
Liability Insurance
Needle Stick and Blood and Body Fluid Policy and Procedure
Policy Against Abusive Conduct
Policy on Student Rights Under the Family Educational Rights and Privacy Act
Research Integrity Policy
Social Media Policy
Student Mistreatment Reporting and Monitoring Policy
Student Organization Alcohol Guidelines
Supporting a Fair Environment
WashU Medicine strongly encourages learners and other community members to immediately report their concerns regarding learner mistreatment or other unprofessional behavior in the learning and working environment via the SAFE Reporting website, without fear of retaliation. The university will strive to protect the confidentiality of persons reporting mistreatment and the individuals involved. Learners may submit a report anonymously if they prefer; however, the university may be limited in its ability to respond and take action on anonymous reports. De-identified aggregate data on reports submitted to SAFE is reported back to the WashU community quarterly.
WashU Medicine Programs Student Mistreatment Reporting and Monitoring Policy (Bulletin)
For additional information, review your SAFE Learning Modules in MyCanvas. If you cannot find the modules, please complete a SAFE Learning Modules Opt-In form.
Gender Equity and Title IX Compliance at WashU
Social Media
Student must read and follow WashU Medicine Social Media Policy. https://marcomm.med.wustl.edu/items/social-media-guide/
Policy on Alcohol in the Program
The Program adheres to the policies of the University on alcohol and drugs. https://sites.wustl.edu/prograds/university-wide-graduate-student-group-handbook/alcohol-policy-for-graduate-student-organizations/
Unauthorized Recording and Distribution of Classroom Activities and Course Materials
Except as otherwise expressly authorized by the instructor or the university, students may not record, stream, reproduce, display, publish or further distribute any classroom activities or course materials. This includes lectures, class discussions, advising meetings, office hours, assessments, problems, answers, presentations, slides, screenshots or other materials presented as part of the course. If a student with a disability wishes to request the use of assistive technology as a reasonable accommodation, the student must first contact the Office of Disability Resources to seek approval. If recording is permitted, unauthorized use or distribution of recordings is also prohibited.
Students’ Rights
The Family Education Rights and Privacy Act (FERPA) can be viewed on the Program’s intranet at: https://registrar.wustl.edu/student-records-resources/ferpa-overview/
Books and Tools
The faculty work regularly to keep the reading of books and assignments limited to what they think is necessary for preparing you for safe clinical practice. The faculty believes the reading for class is critical material that not only reinforces what is lectured on in class but extends the content beyond what can be gained by lecture. Unless it is noted, faculty members consider reading assignments required and they will test on content that is assigned.
Faculty members select required books on the basis of whether they themselves would buy the book for keeping in a personal library. Required books are expected to be useful to students for many years, and not become obsolete in a short period of time. Because students could never rely wholly on what they learn in lecture and what they remember after the program for safe practice, books should be purchased and kept for personal reference. A library is a wise investment that all faculty members value highly.
The faculty have carefully developed a list of clinical tools that they feel are necessary for physical therapists to own for use in the clinic. Students are expected to arrive to the Program with the following list of items and guidelines are provided to incoming students as to the quality and type needed.
Student Responsibility:
- tape measure
- reflex hammer
- pen light
- standard adult pressure cuff
- stethoscope
Program provides at Orientation:
- variety of goniometers
Optional:
- stainless steel scissors
- inclinometer
Level 2 surgical masks, Inclinometers, flexible rulers, gait belts, and scissors are provided for student use while they are in the Program for use during class. They are stored in the equipment closet lockers. Students are responsible for returning all borrowed equipment to the designated lockers.
See the section on clinical education to learn about clinical tools and uniform requirements for the clinical experiences.
Security
Your medical school picture I.D. is required to enter the Medical School buildings and you must wear it at all times. Security guards are posted at the entrance to the 4444 Building from 6:00 a.m. until 10:00 p.m. (M-F) and 6:30 a.m. – 4:30 p.m. on Saturday. On Sundays, security is not in the building. The building is locked, and an ID badge is necessary for entrance. Security also is located in, the Medical School and at Olin Residence Hall. The guards will provide escort service to cars parked on the surface lots or other buildings on the Medical School Campus after dark. The Boulevard Building, the Medical School, and Olin Residence Hall offer 24-hour security. Entrance to the front at night and on weekends is through the south main doors and will require your badge for entrance.
Students have 24-hour access to the Program’s classrooms for studying and lab practice. Students will gain entrance with their WUSM badges. Students are permitted into the classrooms and student lounge at any time. If any of these doors are locked, please call security, 362 –Help (314-362-4357) to request that they be opened. Report any problems with access to the Program rooms to a staff member.
Student Health Services
The Student Health Services team provides students at WashU Medicine School of Medicine with efficient, accessible, high-quality medical care, without undue financial burden, in order to prevent and treat health problems that may interfere with a student’s educational and professional goals while attending WUSM. The Student Health Service is the primary resource for student health care needs. They are conveniently located on campus. They provide a full range of primary care medical services, mental health services, and health promotion and wellness services. Their clinical staff consists of physicians, nurse practitioner, nurses, psychologists, and administrative staff. At Student Health Services, their team is dedicated to fostering a supportive environment where every student’s health and well-being are prioritized, ensuring they can thrive academically and professionally at WashU Medicine School of Medicine. Please call (314) 362-3523 to schedule an appointment.
For more information, including required documentation, frequently asked questions, outpatient care, services on and services away from campus, the student health plan, vaccinations, and exposures, visit:
https://studenthealth.med.wustl.edu/
https://studenthealth.med.wustl.edu/services/mental-health-information/
Disability Resources
Disability Resources – Students (wustl.edu)
Academic Support
For information about tutoring, open labs, and the writing center, please visit Student Commons in Canvas.
Policies for student access to tutoring services are included in the Student Commons course in Canvas, under Educational Resources and Academic Support. Approval for tutoring comes from either the module lead or the Assistant Director of Learning and Continuous Improvement. Tutors are fellow first-, second-, and third-year learners. Tutoring may occur in person or virtually. It is the responsibility of the tutee to reach out to the tutor to schedule tutoring sessions. There is an expectation that if you are paired with a tutor that the resource is used consistently. If a learner decides they no longer with to work with a tutor or if for some reason the tutor/tutee pairing does not work, learners or tutors should contact the Assistant Director of Learning and Continuous Improvement.
Workday
Workday is an application which includes academic records (grades, intent to graduate etc.), billing records (account, pay/view bill, third party billing, etc.), contact information (address/e-mail address), courses and registration (course listings, bulletin etc.), and personal preferences (information restriction/password). You may access Workday at https://workday.wustl.edu/. It is very critical that you update your local address and phone number during orientation and keep it updated so that your financial aid, etc. will be processed in a timely manner.
WashU aims to be a diverse community fully committed to the principles of equity, fairness and inclusive excellence.
For more information and opportunities, see Equity, Diversity & Inclusion
Financial Aid
Office of Student Financial Planning | WashU Medicine (wustl.edu)
Information about Program scholarships can be located in Student Commons.
Safety and Participation Policies in the Program
The purpose of the Safety and Participation Policy is to ensure that students are physically, and emotionally safe to learn in an environment with equipment that is routinely monitored by students, faculty, and the BJC Clinical Engineering Department.
By matriculating and continuing in the Physical Therapy Program, a student agrees that they may be selected by the instructor and used as a model for class demonstration. A student also agrees to work with fellow students as a lab partner for examination and treatment practice. If for any reason a student believes that they have a medical condition, religious restriction or cultural restriction that would prohibit participation, the student has the responsibility to inform the module lead and the Division Director of Education. The student may be required to obtain documentation to verify the above reasons for limited or non-lab participation. In the event of a medical condition, the student may need to seek disability accommodations to ensure that Program Technical Standards can be met. Continuation in the course and program will be determined on an individual basis and the student is required to demonstrate proficiency in performing all skills on a classmate or tester during practical examinations and clinical education experiences as outlined in each course syllabus.
Safety
Being a student in the Physical Therapy Program involves certain activities that pose potential risks. The Physical Therapy Program is committed to the safety of the students. Students must adhere to program policies regarding safety as well as the following issues related to safety in the classroom and lab:
- Students must demonstrate appropriate safe, ethical, and professional behavior as well as didactic course competence to progress through the physical therapy program. Unsafe, unethical, or unprofessional behavior may prevent a student from successfully completing a didactic or clinical course.
- All program equipment undergoes an annual safety and calibration check. In addition, students and faculty are responsible for monitoring all equipment for signs of wear and malfunction. Any equipment demonstrating a safety concern will be immediately removed from student use and the Division Director of Education will be notified.
- Students are responsible for prompt reporting of any acute adverse health event (injury or illness) associated with a class or lab session to the module lead, or in the event of an adverse health event during a clinical education experience, to the Associate Director of Clinical Education. If needed, 314-362-4357 (2-Help) should be called and the faculty member in charge will be responsible for completing an incident report as described in the Emergency Organization information.
- It is the responsibility of the student to report relevant health information to the module lead when it results in the student not being able to perform a lab activity or serve as a lab partner. A written note from a physician may be required outlining specify activity precautions or guidelines.
- In order to provide an optimal learning environment which is safe and clean, students are expected to participate in routine classroom cleaning procedures following the completion of each class and lab.
- Students are expected to follow appropriate Hazardous Material and Infection Control Policies as trained during each year’s orientation and appropriate to the environment whether it be in the classroom, laboratory, or clinical setting. Students are required to follow Universal Precautions. All blood and body fluids are treated as if known to be infectious for blood borne pathogens. Gloves, masks and gowns are available on-site and frequent use of hand sanitizer and hand washing is required.
- First aid kits, fire extinguishers and AEDs are located on each floor of the program. Please refer to the Emergency Organization information for specific locations.
- Specific policies and procedures are discussed in courses throughout the program. Any questions about safety should be directed to the appropriate faculty member and the Division Director of Education.
Emergency Preparedness
The emergency classroom plan, emergency preparedness procedures, emergency coordinator list, and incident report can all be located in Student Commons.
International Travel
Policies and Recommendations for International Travel
WashU’s International Travel Oversight Committee (ITOC) provides policy for international travel conducted by students, faculty, postdoctoral trainees, clinical fellows, and staff of WashU.
https://global.wustl.edu/resources/international-trave
The Federation of State Boards of Physical Therapy (https://www.fsbpt.org) administers the physical therapy licensure exam. A license is required to practice physical therapy; it is illegal to practice without a license and doing so can influence future licensure as well. While the licensure exam is the same for every state, each state (or compact) has its own licensing law and procedures. Graduates may only apply for licensure in one state at a time, and each state has its own fees for application. When licensure is desired in more than one state, one must pass the national licensure exam and be licensed in one state before being permitted to apply for reciprocity in another state. Although the applicant does not have to repeat the exam, there is a fee in every state for reciprocity. Graduates are responsible for learning the licensure requirements in their states or compact license.
Some states allow graduates to practice under a temporary license, which is issued after successful application to take the exam has been made and before actually taking the exam. Temporary licenses are valid only for a limited time. Many states are now requiring a written statement from applicants (and those renewing their licenses) indicating they are physically and emotionally fit to practice. If a state has reason to believe that a graduate is not fit to practice or has a history that puts him or her at risk for future fitness, that state may impose certain conditions on licensure (e.g. monitoring by a psychiatrist in the event of current or past emotional difficulties).
Generally, to apply for licensure as a physical therapist, students need to have graduated from an accredited program in physical therapy. Proof of graduation most often includes having your diploma. Some states accept attestation letters from the Program prior to graduation. The Program will provide attestation letters for only students who are in good standing and on track to graduate at an expected time. Students are not encouraged to take the board exam prior to graduation due to the risk that studying for the exam could compromise their academic performance during the fifth semester. However, there are times when a student may request to take the exam prior to graduation due to a residency application timeline or other personal situation. Below are the criteria for when the program will provide attestation prior to graduation.
- Students must be in good standing and on track to graduate at an expected time.
- Students must score a 600 or above on the Academic PEAT.
The Academic PEAT is administered by the Program during Module 7. A score obtained by a student on their own is not acceptable to demonstrate the minimum score required for attestation. The program approves any requested early attestation letters after the Module 7 PTCAC meeting.
Students should be aware that it is unlawful to share in any way what is included on the national exam. Students should only use official website offers from the FSBPT for obtaining sample questions and study advice. Students should be aware that other study guides are commercially prepared and are not official.
Students also need to be aware that any violation of the law, beyond parking tickets and moving violations may be cause for special review by the licensing board or refusal to take the board exam. Graduation from the Program does not guarantee that a graduate will be eligible to take the licensure exam.
Information about licensure can be found in Student Commons.
The faculty of the Program in Physical Therapy is committed to a flexible curriculum – one which changes with the needs of the profession and the needs of the students. A major source of information that contributes to the changes made in the program is constructive feedback from students and graduates.
You will be asked to participate in this process to assess the effectiveness of examinations, courses, including clinical education, and collections of courses. Though changes cannot always be made immediately, the faculty regards all feedback when making decisions. You can have an impact on the program in the future. We ask you to be diligent in giving us feedback so that we can continue to improve our curriculum. Students should sign all evaluation forms to give credibility to their comments.
Data from the evaluations are summarized and shared with those who are appropriate to receive it. All faculty members receive general semester feedback summaries. All module teams receive summaries of feedback pertaining to their specific module. Lecturers, lab assistants, and coaches receive all feedback submitted on them. The Division Director of Education reviews all feedback.
Examination Evaluations: Students have the option of critiquing each written and practical examination given. Written test feedback can be provided within ExamSoft. Performance exam evaluations will be provided at the end of each performance assessment. Evaluations are optional.
Semester and Annual Evaluations: Learners have the opportunity to provide feedback through module evaluation surveys, lab assistant evaluation surveys, focus groups, coach program evaluation surveys, and belongingness surveys.
End of Program Evaluation: Just prior to graduation, learners are provided the opportunity to complete an end of the program evaluation.
Graduate Survey: Approximately one year after graduation alumni receive a final survey, which allows them to comment on the program and their current practice.
WashU encourages and gives full consideration to all applicants for admission, financial aid, and employment. The University does not discriminate in access to, or treatment or employment in, its programs and activities on the basis of race, color, age, religion, sex, sexual orientation, gender identity or expression, national origin, veteran status, disability or genetic information. Inquiries about compliance should be addressed to the University’s Vice Chancellor for Human Resources, WashU, Campus Box 1184, One Brookings Drive, St. Louis, MO 63130.